

Vaginal Birth After Cesarean Delivery
- Author: Aaron B Caughey, MD, MPH, PhD; Chief Editor: Carl V Smith, MD more...
- Sections Vaginal Birth After Cesarean Delivery
- Preparation
- Post-Procedure
“Once a cesarean, always a cesarean.” From 1916, when these words were spoken to the New York Association of Obstetricians & Gynecologists, through the ensuing 50-60 years, this statement reflected most of US obstetricians’ management of patients with a prior cesarean delivery . By 1988, the overall cesarean delivery rate was 25%, rising from less than 5% in the early 1970s. Only 3% of live-born infants were delivered vaginally after the mother had undergone a prior cesarean delivery.
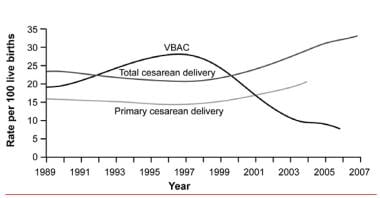
Although attempts at a trial of labor after a cesarean birth (TOLAC) have become accepted practice, the rate of successful vaginal birth after cesarean delivery (VBAC), as well as the rate of attempted VBACs, decreased during a 10-year period (see the image below). Whereas 40-50% of women attempted VBAC in 1996, as few as 20% of patients with a prior cesarean delivery attempted a trial of labor in 2002. This number drifted down toward the 10% mark, with fewer than 10% of women achieving successful VBAC in 2005. More recent data show that from 2016 to 2018, rates of VBAC in the United States rose from 12.4% in 2016 to 12.8% in 2017 and to 13.3% in 2018. [ 1 ]
Despite the known risks (0.5-1% rate of uterine rupture), TOLAC remains an attractive option for many patients and leads to a successful outcome in a high proportion of cases. In comparison, the alternative of elective repeat cesarean delivery is not without risks. In addition to the inherent risks that cesarean delivery has over vaginal delivery, patients may experience uterine rupture prior to the onset of labor.
The decision to undergo TOLAC is an individual one that should be based on careful, thorough counseling. [ 2 ] Maternal characteristics and obstetric history can provide a patient a rough estimate of her chance of a successful trial of labor. This same obstetric history can be used to estimate a patient’s risk of uterine rupture.
If possible, avoid induction of labor, because induction of labor decreases the probability of success and increases the chance of uterine rupture in a trial of labor after cesarean delivery. Counsel patients who elect to undergo TOLAC to be evaluated early in labor and to manage the pregnancy in a hospital setting in which uterine rupture can be both recognized and managed expediently.
Certainly, counseling should address the question of whether patients are interested in subsequent pregnancies after the current pregnancy. Undergoing 2 prior cesarean deliveries further increases the risks of VBAC in a subsequent pregnancy; thus, for a future pregnancy, having had a successful VBAC offers protection after undergoing the risk in the current pregnancy.
Go to Cesarean Delivery and Perimortem Cesarean Delivery for complete information on these topics.
ACOG guidelines
Several factors contributed to a decline in VBAC. As practitioners experience complications related to managing patients undergoing trials of labor after cesarean delivery, they are less likely to allow new patients to undergo a trial of labor. In addition, 1999 guidelines from the American College of Obstetricians and Gynecologists (ACOG) stated explicitly that patients undergoing TOLAC require the presence of an obstetrician, an anesthesiologist, and/or a staff capable of performing an emergency cesarean delivery throughout the patient’s active phase of labor. [ 3 ]
Whereas academic centers and larger community hospitals are able to comply with these requirements, many smaller hospitals do not offer in-house anesthesia or obstetric staff. Furthermore, to meet the financial demands of managed care, many obstetricians now cover more than one hospital simultaneously, making it difficult to comply with the 1999 guidelines.
The impact of these changes can be observed in national birth statistics. The cesarean delivery rate peaked at 25% in 1988 but then declined to 21% overall in 1996. From 1996 to 2004, however, the cesarean delivery rate increased to 29.2%, while the rate of VBAC declined from 28% to 9%. On the assumption that the overall VBAC success rate is about 70%, this correlates with a decline from 40% to 14% in the number of patients choosing to undergo TOLAC.
What once was hailed as a key component of lowering the overall cesarean birth rate (ie, TOLAC) is losing the support it had in the 1980s. Overall, this has led to a rate of cesarean delivery of 31.1% in 2006, which is the highest rate in US history and shows no signs of decreasing.
In 2010, with these developments in mind, ACOG issued new guidelines that were somewhat less restrictive. [ 4 , 5 ] The 2010 guidelines, based on consensus and expert opinion, recommend that TOLAC should be undertaken at facilities capable of emergency deliveries. Because of the risks associated with TOLAC and complications such as uterine rupture that may be unpredictable, ACOG recommends that TOLAC be undertaken in facilities with staff immediately available to provide emergency care.
However, when resources for immediate cesarean delivery are not available, health care providers and patients considering TOLAC should discuss the hospital’s resources and availability of obstetric, pediatric, anesthetic, and operating room staffs. Respect for patient autonomy supports allowing patients to accept increased levels of risk; however, patients should be clearly informed of such potential increase in risk and counseled about management alternatives.
Recognizing that TOLAC was decreasing at community and more rural hospitals, ACOG revised these recommendations in 2017 with an apparent goal in softening the recommendation for immediate availability of surgical teams. The language now reads "ACOG recommends that TOLAC be attempted in facilities that can provide cesarean delivery for situations that are immediate threats to the life of the woman and the fetus". This more nuanced statement may result in an increase in attempted TOLAC at these facilities. [ 6 ]
On the basis of level A evidence, the 2017 ACOG guidelines make the following recommendations [ 6 ] :
Most women with a prior cesarean delivery with a low transverse incision are candidates for VBAC and should be offered TOLAC.
Epidural anesthesia may be used as part of TOLAC.
Misoprostol should not be used for patients who have had a prior cesarean delivery or major uterine surgery.
On the basis of level B evidence, TOLAC may be considered for the following patients [ 6 ] :
Women with 2 previous low transverse cesarean deliveries
Women with 1 previous cesarean delivery with a low transverse incision who are otherwise appropriate candidates for twin vaginal delivery
Women with 1 previous cesarean delivery of unknown incision type, unless clinical suspicion of a previous classical uterine incision is high
Women with 1 previous cesarean delivery who are otherwise appropriate candidates for twin vaginal delivery.
Level B evidence was also found for the following:
Induction of labor during TOLAC is not contraindicated.
In women with a prior low transverse uterine incision who are at low risk for adverse maternal or neonatal outcomes from external cephalic version and TOLAC, external cephalic version for breech presentation is not contraindicated.
Continuous fetal heart rate monitoring is recommended during TOLAC
A comparison of VBAC in the United States, the United Kingdom, and Canada showed understandable similarities but numerous unexplained differences in recommendations. [ 7 ]
Outcomes of interest
Two specific outcomes of interest regarding TOLAC have been well investigated: successful VBAC and uterine rupture. Other outcomes are certainly of interest, including neonatal outcome, hysterectomy, and maternal mortality; however, few studies have focused on these outcomes, and poor outcomes occur too rarely to be well represented in established databases.
In earlier studies, most outcomes were reported after univariate analysis. Risk factors were examined without controlling for potential confounding variables, and results were reported as a relative risk or odds ratio. These ratios represent the risk of the group of individuals who have the risk factor divided by individuals without the risk factor. Over the last decade, several large cohorts have examined predictors and outcomes related to women with a prior cesarean delivery. These studies have ranged from Nova Scotia to Boston to the state of Washington.
Finally, 2 large multicenter studies have been publishing multiple studies on this issue, one out of Pennsylvania and the other out of the Maternal-Fetal Medicine Units. These large studies over the last decade have used multivariate statistics to examine risk factors. This means that other risk factors and confounding factors, such as birth weight, maternal age, obstetric history, and labor management, were controlled for in the analysis.
In this article, factors associated with mode of delivery in the setting of a trial of labor and factors associated with uterine rupture in this same setting are reviewed.
Indications
The predictors of successful TOLAC are extensively described in the existing literature (see the table below). Although no randomized trials have been conducted, relatively large databases have been analyzed (with both univariate and multivariate techniques) to determine risk factors for patients undergoing TOLAC.
In addition, several scoring systems have been devised to help predict which patients are likely to be successful when attempting VBAC. These scoring systems are quite varied and may inform the discussion with the patient about TOLAC. However, there are no prospective studies that demonstrate that these systems improve perinatal outcomes. Examples of these calculators can be found on the ACOG website. The Eunice Kennedy Shriver National Institute of Child Health and Human Development VBAC Calculator was updated in 2021 to remove race and ethnicity as a predictor and to add the variable of chronic hypertension treated with medication. [ 8 ] ACOG emphasizes that a VBAC calculator score should not be used as a barrier to TOLAC; it is one of many tools that can be used to inform shared decision-making. [ 9 ]
Table 1. Predictors of VBAC Success or Failure (Open Table in a new window)
|
|
Prior vaginal delivery | Maternal obesity |
Prior VBAC | Short maternal stature |
Spontaneous labor | Macrosomia |
Favorable cervix | Increased maternal age (>40 y) |
Nonrecurring indication (breech presentation, placenta previa, herpes) | Induction of labor |
Preterm delivery | Recurring indication (cephalopelvic disproportion, failed second stage) |
| Increased interpregnancy weight gain |
| Latina or African American race/ethnicity |
| Gestational age ≥41 wk |
| Preconceptional or gestational diabetes mellitus |
Because no large, prospective, randomized, controlled trials have been conducted, most of the risk factors have been determined from retrospective cohort and case-control studies. These studies have been increasingly analyzed with multivariate techniques to control for confounding factors. However, control for physician practice is difficult, and physician practice can greatly impact the strength of the association between these risk factors and a successful VBAC.
Even when demographic data, obstetric history, birth weight, gestational age , induction of labor, and other variables are controlled for, the bias inherent in nonrandomized and nonblinded trials cannot be eliminated.
Maternal characteristics
Several studies examine prepregnancy weight and height to examine the effect on mode of delivery. Not surprising, women who are shorter and women who are obese are more likely to undergo cesarean delivery. Of note, cesarean delivery has been associated not only with increased prepregnancy weight but also with increased gestational weight gain.
An increasing number of studies have been carried out in the setting of TOLAC, all of which show that women in the morbidly obese range have a higher risk of failing a trial of labor. Interpregnancy weight gain has been shown to increase the risk of failure in a subsequent trial of labor, but unfortunately, interpregnancy weight loss has not demonstrated an improvement in VBAC success.
Maternal age has also been examined in several studies in VBAC literature. With confounding factors adjusted for, women older than 40 years who have had a prior cesarean delivery have an almost 3-fold higher risk for a failed trial of labor than do women younger than 40 years. In 1 scoring system, women younger than 40 years were given an extra point as a predictor for successful VBAC. [ 10 ]
Maternal race or ethnicity has been examined as a predictor for VBAC in the setting of trial of labor and has not generally been noted to be a strong predictor. However, in the recent Maternal-Fetal Medicine Unit (MFMU) Cesarean Registry, both Hispanic ethnicity and African American ethnicity were associated with lower rates of successful trial of labor. Whether this association is due to actual biologic reasons or whether ethnicity is acting as a proxy for some other factor or factors remains to be elucidated.
Birth weight
Birth weight greater than 4000 g is associated with an almost 4-fold higher risk of cesarean birth among nulliparous women. Several studies have demonstrated a difference in VBAC rates between patients with a birth weight greater than 4000 g and those with a lower birth weight. In accordance with these findings, several studies have demonstrated a higher failure of a trial of labor with increasing birth weight.
Obstetric history
Obstetric history is enormously important in terms of risk factors for successful TOLAC. Predictors of increased success include a nonrecurring indication for prior cesarean delivery (eg, breech presentation, placenta previa) and prior vaginal delivery. A history of cephalopelvic disproportion (CPD), failure to progress, no prior vaginal deliveries, or a prior cesarean delivery performed in the second stage of labor are negative predictors of success in a subsequent trial of labor.
Several studies have examined indications for prior cesarean delivery as a predictor of outcome in subsequent TOLAC. In all studies, CPD had the lowest VBAC success rate (60-65%). Fetal distress (eg, nonreassuring fetal testing) had the second lowest success rate of VBAC (69-73%). Nonrecurrent indications, such as breech birth, herpes, and placenta previa, were associated with the highest rates of success (77-89%).
Failure to progress, CPD, or dystocia as indications for prior cesarean delivery are also associated with a higher proportion of patients not attempting a trial of labor after cesarean birth. In a meta-analysis of the existing literature prior to 1990, Rosen et al demonstrated that women whose prior cesarean delivery was performed for CPD were twice as likely to have an unsuccessful trial of labor. [ 10 ]
Patients with a prior vaginal delivery have higher rates of successful VBAC than patients without a prior vaginal birth. Furthermore, women with a successful VBAC have a higher success rate in a subsequent trial of labor compared with women whose vaginal delivery was prior to cesarean delivery.
In an unadjusted comparison, patients with 1 prior vaginal delivery had an 89% VBAC success rate compared with a 70% success rate in patients without a prior vaginal delivery. In comparable comparisons controlling for confounding factors, odds ratios of 0.3-0.5 for rate of cesarean delivery are found. Among patients with a prior VBAC, the success rate is 93%, compared with 85% in patients with a vaginal delivery prior to their cesarean birth but no prior VBAC. These findings have been repeatedly validated by multiple studies.
Only 1 study carefully examines cervical dilation at prior cesarean delivery. In this study, the degree of cervical dilation in the prior delivery is directly associated with the likelihood of success in a subsequent trial of labor. For example, 67% of patients who were dilated 5 cm or less at the time of their delivery had a successful VBAC, compared with 73% of patients who were dilated 6-9 cm.
The success rate is much lower for patients whose labor arrested in the second stage: only 13% of patients who were fully dilated at the time of their prior delivery had a successful VBAC. In a similar study, patients who had their prior cesarean delivery in the first stage of labor had a lower rate of cesarean delivery than those who had their prior cesarean delivery in the second stage of labor. However, in this study, 66% of patients who had a cesarean delivery for dystocia in the second stage had a successful VBAC.
Induction of labor
Patients who undergo induction of labor are at a higher risk of cesarean delivery than women who experience spontaneous labor. This finding has also been observed in women with a prior cesarean delivery. Several studies have demonstrated that women who are induced in TOLAC have a 2- to 3-fold increased risk of cesarean delivery compared with those who present with spontaneous labor.
One study demonstrated that patients who could be induced with oxytocin had a significantly lower cesarean delivery rate compared with those induced with a Foley bulb.
The 2017 ACOG guidelines state that induction of labor for maternal or fetal indications remains an option in women undergoing TOLAC. [ 6 ]
Gestational age
Increasing gestational age is associated with a decreased rate of successful VBAC. Three potential factors are related to the association of increasing gestational age with an increased rate of cesarean delivery: increasing birth weight, increased risk of fetal intolerance of labor, and increased need for induction of labor. However, in a recent study that controlled for both birth weight and induction/augmentation of labor, gestational age of greater than 41 weeks was still associated with failed VBAC.
Cervical examination on admission
Not surprisingly, patients who present to labor and delivery with advanced cervical examination findings have a greater success rate of vaginal birth. Several components of the cervical examination have been investigated, including cervical dilation and cervical effacement. Not surprisingly, the more advanced the cervical examination finding is upon initial presentation, the higher the rate of successful VBAC. A 1997 Flamm et al study demonstrated that patients presenting with dilation greater than or equal to 4 cm had an 86% rate of VBAC. [ 11 ]
Interpregnancy interval
The timing between pregnancies has recently become an interesting predictor for a number of obstetric outcomes, VBAC success among them. In 1 analysis, women who had an interpregnancy interval of more than 18 months had an 86% chance of VBAC success, while women whose interpregnancy interval was less than 18 months had a VBAC success rate of 79%. This difference was not statistically significant, and it remains unclear whether the interpregnancy interval actually affects the success rate or whether it affects only the risk of uterine rupture.
Preterm delivery
Preterm labor and delivery deserves attention as an opportunity to recounsel women about the risks and benefits of a trial of labor after cesarean delivery. In a large study by Quinones et al, 12,463 attempted a trial of labor, and the VBAC success rates for the term and preterm groups were 74% and 82%, respectively. [ 12 ] Additionally, a trend toward decreased risk of uterine rupture among preterm delivery gestations was found. These data can certainly be used to counsel women with a prior cesarean who are in preterm labor.
Gestational or pregestational diabetes
Only 1 study of patients undergoing a trial of labor after cesarean delivery has examined the rate of success in patients with diabetes mellitus (DM). This study demonstrated that patients with either gestational DM or pregestational DM had a lower rate of successful trial of labor. These findings are not particularly surprising; however, further studies are needed to sort out the differences between gestational and pregestational DM and the interaction between DM and birth weight.
Contraindications
One of the most significant risks women face when considering a trial of labor is that of uterine rupture. This potentially fatal event may have significant maternal and neonatal sequelae.
A threshold of acceptable risk has been established between the risk reported in women with 1 prior cesarean delivery (0.5-1%) and that seen in women with a history of a prior classic cesarean delivery (6-12%). The latter patients, along with women who have undergone metroplasties for uterine anomalies or myomectomies that have entered the uterine cavity, are discouraged from attempting VBAC.
Other patients who are at increased risk for uterine rupture include those who have had 2 or more hysterotomies, those who are treated with prostaglandin agents, and those undergoing induction of labor (see the table below).
Table 2: Predictors of Uterine Rupture (Open Table in a new window)
|
|
Classic hysterotomy | Spontaneous labor |
Two or more cesarean deliveries | Prior vaginal delivery |
Single-layer closure | Longer interpregnancy interval |
Induction of labor | Preterm delivery |
Use of prostaglandins |
|
Short interpregnancy interval |
|
Infection at prior cesarean delivery |
|
Nature of hysterotomy
Unquestionably, practitioners do not feel safe allowing a patient who has had a prior classical hysterotomy (ie, a vertical incision that has extended above the insertion of the round ligaments) to undergo TOLAC. Patients with a prior classical hysterotomy have a higher rate of uterine rupture in subsequent pregnancies. Because these patients can sustain a uterine rupture prior to labor, they are often delivered at 36-37 weeks’ gestation. Although available data are limited, the risk of uterine rupture in this group of patients is estimated at 6-12%.
Retrospective cohort studies have demonstrated that the risk of uterine rupture is no greater for patients who have had a vertical incision in the lower uterine segment than for those who have had a transverse incision. The rate of uterine rupture from these studies is 0.8-1.3%. When comparing patients with prior Krönig hysterotomies to patients with low transverse incisions, no statistical difference exists in either univariate or multivariate analyses controlling for the confounding factors of obstetrical history, induction of labor, birth weight, and length of labor.
Most babies delivered abdominally are delivered through a transverse incision in the lower uterine segment (Kerr hysterotomy). In several large retrospective cohort studies, the reported rate of uterine rupture is 0.3-1% (see the table below). [ 13 , 14 , 15 , 16 , 17 , 18 ] Rates of 0.5-1% (1 in 200 to 1 in 100) are commonly used to counsel patients with no other additional risk factors.
Table 3: Rates of Uterine Rupture (Open Table in a new window)
|
|
| |
Miller (1994) | 10,880 | 63 (0.6%)* | |
Flamm (1994) | 5,022 | 39 (0.8%) | |
McMahon (1996) | 3,249 | 10 (0.3%) | |
Shipp (1999) | 2,912 | 28 (1%) | |
Landon (2004) | 17,898 | 124 (0.7 %) | |
Macones (2005) | 13,331 | 128 (0.9%) | |
*Includes unknown | |||
When an operative report of a patient’s prior cesarean delivery is unavailable, the obstetric history may be helpful in determining the type of uterine incision. For example, a patient who underwent a cesarean delivery for a breech presentation at 28 weeks’ gestation has a much higher risk of a vertical uterine incision than the patient at term with arrest of dilation. Because most cesarean deliveries are via low transverse hysterotomies, the risk of uterine rupture for patients with an unknown uterine scar is usually similar to that of patients with a prior transverse incision.
Several studies examining this issue have demonstrated that the rate of rupture for patients with an unknown uterine incision is approximately 0.6%. A case-control study of patients with and without uterine rupture did not find unknown hysterotomy to be a risk factor compared with low transverse hysterotomy. [ 19 ]
According to the 2017 ACOG guidelines, TOLAC is not contraindicated for women with previous cesarean delivery with an unknown uterine scar type unless clinical suspicion of a previous classical uterine incision is high. [ 6 ]
Number of prior cesarean deliveries
Patients with more than 1 prior cesarean delivery are at increased risk of uterine rupture. The unadjusted rate of uterine rupture for patients with 2 prior uterine incisions ranges from 1.8% to 3.7%.
One analysis demonstrated that when potential confounding variables (eg, prior vaginal delivery) are controlled for, patients who have had 2 prior cesarean deliveries have 5 times the risk of uterine rupture compared with patients who have had only 1 prior cesarean delivery. This finding contradicted several earlier studies that did not control for confounding factors, most importantly prior vaginal delivery.
More recently, a study that examined major complications overall found that while there was a statistically significant increase, the adjusted odds ratio was only 1.6.
Type of uterine closure
Whereas the uterine hysterotomy had traditionally been closed in several layers, in the 1990s physicians at many institutions began closing the Kerr hysterotomy in a single layer. Because the lower uterine segment is quite thin, a single layer often afforded adequate hemostasis. Several recent studies have compared women whose hysterotomy was closed in a single layer with those whose hysterotomy was closed in 2 layers. Adjusted odds ratios of 3 to 4 for uterine rupture have been estimated for women who have a single-layer closure.
Prior vaginal delivery
Prior vaginal delivery appears to be protective for subsequent uterine rupture. A 2000 study by Zelop et al demonstrated that patients with a prior vaginal delivery had a 0.2% rate of rupture compared with 1.1% for patients with no prior vaginal delivery. An adjusted odds ratio controlling for confounding factors was 6.2. [ 20 ]
No studies have compared the rate of uterine rupture in patients with a prior VBAC with those with a vaginal delivery before their prior cesarean delivery. These findings have been validated in subsequent studies, though the effect size has not been quite as large.
Prior infection
A recent study demonstrated that women who had an infection at the time of the cesarean delivery have an increased rate of uterine rupture in a subsequent trial of labor. The assumed causal mechanism is poor healing of the hysterotomy secondary to the infection.
While labor appears to be a risk factor for uterine rupture, many patients experience a uterine rupture prior to the onset of labor. In a large study using birth certificate data, one study found that the rate of uterine rupture before the onset of labor was 0.5%. Patients at greatest risk are those with prior classical hysterotomies. As a result of this potential risk, these patients are usually scheduled for delivery at 36-37 weeks’ gestation.
When counseling this group of patients, however, mentioning that scheduling an early repeat cesarean delivery does not eliminate the risk of uterine rupture entirely is important.
Induction of labor as a risk factor for uterine rupture has been examined over only the past 5 years. One large study, which did not control for confounding factors, demonstrated a uterine rupture rate of 2.3% in patients who had experienced induced labor. In several studies controlling for confounding factors, adjusted odds ratios were 2-4 for patients who were induced compared with those who presented in spontaneous labor.
Despite these analyses, discerning whether induction of labor itself leads to uterine rupture or whether another risk factor (as yet unmeasured) is associated with both induction of labor and uterine rupture is difficult. When patients have an indication for induction of labor, the best course of management is to discuss the increase over their baseline risk of uterine rupture.
Use of oxytocin
In the only prospective randomized trial in women with a prior cesarean delivery, oxytocin augmentation in early labor was compared with expectant management; 5 uterine ruptures occurred in the augmentation group (5%), and none occurred in the expectant management group. Excessive use of oxytocin has been described as leading to an increased risk of uterine rupture.
A 1993 study by Leung et al demonstrated an odds ratio of 2.7 for uterine rupture in patients who used oxytocin compared with those without oxytocin augmentation. [ 19 ] However, this study included inductions and augmentation in both the latent and active phases. These confounding factors may have contributed to much of the difference because induction of labor alone has an increased risk.
In 2 subsequent studies, oxytocin augmentation was associated with uterine rupture. [ 21 , 13 ] In the first study, although the odds ratio was 2.3, it was not statistically significant, probably because of inadequate statistical power. In the latter study, a similar odds ratio of 2.4 existed.
Because labor and delivery units use oxytocin widely, this oxytocin–uterine rupture relationship deserves careful consideration; the relationship directly affects management of patients. At this point, using oxytocin for induction and augmentation is probably advisable only when absolutely necessary.
Use of prostaglandins
Evidence regarding the use of prostaglandins for induction of labor remains scant. However, in the few trials that have been conducted, the trend is toward an increase in the rate of uterine rupture. In 1999, the use of prostaglandin E2 was demonstrated to have an adjusted odds ratio of 3.2. This study controlled for induction of labor, which appears to be an independent risk factor.
In 2001, Lydon-Rochelle et al demonstrated a 3-fold increase in the risk for uterine rupture when comparing patients induced with prostaglandins with those induced with oxytocin. [ 22 ] In the 2004 study by Landon et al, this effect of prostaglandin induction versus other means was smaller—less than 2-fold (odds ratio of 3.95 with prostaglandin, 2.48 without prostaglandin). [ 13 ]
As in studies examining the risk of uterine rupture in patients undergoing induction of labor, patients who were treated with prostaglandins were likely to have other confounding variables that were not controlled.
In particular, the prostaglandin misoprostol has been examined in small studies. In 1998, Wing et al reported a case series of 17 patients who were induced with misoprostol, in which 2 uterine ruptures occurred. These findings have led to the decreased use of prostaglandins for induction, particularly misoprostol. [ 23 ]
Use of transcervical Foley bulb
Only one small study exists of patients with a prior cesarean being induced with the transcervical Foley bulb. In that study, the rate of uterine rupture was 1.1% with spontaneous labor, 1.2% with induction with amniotomy, and 1.6% with use of a transcervical Foley bulb. This rate is lower than some of the reported rates with prostaglandins, but it is unclear whether the increase seen in patients requiring cervical ripening is due to the need for cervical ripening or to the agents themselves.
Several studies have demonstrated that the shorter the amount of time between the cesarean delivery and the subsequent delivery, the higher the rate of uterine rupture. Commonly, thresholds of 18 and 24 months have been examined. Adjusted odds ratios range from 2.5 to 3 for an increased rate of uterine rupture in the women with less time between deliveries. The biologic plausibility of this effect is related to the amount of time required for the uterine scar to heal completely.
Twin gestations
A study by Cahill et al revealed that whereas women with twin gestations are less likely to undergo a trial of labor after prior cesarean, they appear to be at no increased risk for uterine rupture. [ 24 ]
Other smaller studies examined the rate of uterine rupture in patients with twin gestation undergoing a trial of labor after cesarean delivery, and none of them demonstrated a frank rupture—though when their data were combined, 5 asymptomatic dehiscences in 151 patients were identified. [ 25 , 26 , 27 ]
The rate of asymptomatic uterine dehiscence in patients undergoing a trial of labor after cesarean delivery is difficult to assess because it is not commonly investigated. Thus, although the overall statistical power of the studies examining this issue in twins is not overwhelming, there is certainly no evidence suggesting a higher risk of uterine rupture in these women.
The 2017 ACOG guidelines state that TOLAC may be considered in women with one previous cesarean delivery with a low transverse incision, who are otherwise appropriate candidates for twin vaginal delivery. [ 6 ]
Mullerian anomalies
In 1999, a small series by Ravasia et al examined patients with müllerian anomalies undergoing a trial of labor after cesarean delivery and reported 2 uterine ruptures among 25 patients (8%). [ 28 ] However, both patients with uterine rupture had undergone induction with prostaglandins; therefore, it is difficult to reach any firm conclusions about the relative risk of uterine rupture in this group of patients. The sample size in this study was certainly too small to consider particular types of uterine anomalies.
Patients with prior cesarean deliveries require special management, both antenatally and in labor and delivery. Early in their prenatal care, catalogue patients’ preexisting risk factors for both successful vaginal birth after cesarean delivery (VBAC) and uterine rupture. If uncertain about the prior hysterotomy facts, obtain the operative notes from patients’ cesarean delivery.
When a full obstetric history has been obtained, counsel patients regarding the risks and benefits of undergoing a trial of labor after cesarean delivery (TOLAC), and plan the particular mode of delivery with patients. Some providers and hospitals have particular consent forms for TOLAC that must be signed at this point.
Once the patient presents to the labor and delivery unit and is in labor, it is advisable to go through the risks and benefits of a trial of labor after cesarean delivery (TOLAC) once again. Because of possible changes in the patient’s status, these risks may have changed from the prenatal setting.
For example, if the patient presents in active labor, it seems that both her chances of failed vaginal birth after cesarean delivery (VBAC) and her risk of uterine rupture decrease. In contrast, if she is presenting for induction of labor, her chances of failed VBAC and uterine rupture both increase.
Regarding management on labor and delivery, several practices can help minimize the maternal and neonatal risk. In accordance with the guidelines of the American College of Obstetricians and Gynecologists (ACOG), have an obstetrician, anesthesiologist, and operating room team immediately available to carry out an emergency delivery.
Clinically, observe the patient closely for signs of uterine rupture. Harbingers of uterine rupture include the following:
Acute abdominal pain, persistent beyond contractions
A popping sensation
Palpation of fetal parts outside the uterus upon Leopold maneuvers
Repetitive or prolonged fetal heart rate deceleration
High presenting part upon vaginal examination
Vaginal bleeding
Treat any of these findings as a possible uterine rupture until another source for the finding has been identified. Rupture necessitates immediate delivery.
Expected outcomes
In counseling a patient with respect to the tradeoffs between a trial of labor after cesarean delivery (TOLAC) and an elective repeat cesarean delivery, several factors should be weighed. The rate of success is important: it has been demonstrated that maternal outcomes are better with successful TOLAC than with elective repeat cesarean delivery but are worse with a cesarean delivery after failed TOLAC.
A 2004 study by Landon et al found that the overall measure of morbidity was higher among women who underwent TOLAC. [ 13 ] However, among the 15,801 women who elected to have a repeat cesarean delivery, 2 maternal deaths were reported. Among the 17,898 who underwent a trial of labor, no maternal deaths due to TOLAC or uterine rupture were reported. This difference was too small to be statistically significant; however, the risk of repeat cesarean delivery to maternal morbidity and mortality should be considered.
The other important factor to consider in the setting of TOLAC or a uterine rupture is the neonatal outcomes. A large population-based study from Scotland determined that among 15,515 patients who underwent TOLAC, 7 perinatal deaths occurred as a result of uterine rupture, for a rate of 4.5 per 10,000 women. In comparison, there were no perinatal deaths due to uterine rupture among women undergoing elective repeat cesarean delivery, and the mortality rate was 0.5 per 10,000 among women laboring with no prior cesarean delivery.
A subsequent study demonstrated that among 15,338 patients at term undergoing TOLAC, there were 2 neonatal deaths and 7 cases of hypoxic-ischemic encephalopathy, for rates of 1.4 per 10,000 and 4.6 per 10,000, respectively. [ 13 ] In this series, 114 uterine ruptures occurred among these patients, yielding a neonatal death rate of 1.8% and a hypoxic-ischemic encephalopathy rate of 6.2% in patients with uterine rupture.
Finally, an important individual factor that may tip the scales for many women making the decision about whether to undergo TOLAC is whether they wish to have future pregnancies beyond the current one. Once a vaginal birth has been achieved, both the chances of future success and the risks of uterine rupture are higher.
Furthermore, with each subsequent cesarean delivery, the risks of maternal morbidity and, potentially, maternal mortality increase. Thus, for a woman who wants more children, opting for TOLAC in the current pregnancy may hold more long-term benefits than it would for a woman who is planning on a tubal ligation after delivery.
Osterman MJK. Recent Trends in Vaginal Birth After Cesarean Delivery: United States, 2016-2018. NCHS Data Brief . 2020 Mar. 1-8. [QxMD MEDLINE Link] . [Full Text] .
Studsgaard A, Skorstengaard M, Glavind J, Hvidman L, Uldbjerg N. Trial of labor compared to repeat cesarean section in women with no other risk factors than a prior cesarean delivery. Acta Obstet Gynecol Scand . 2013 Aug 21. [QxMD MEDLINE Link] .
ACOG practice bulletin. Vaginal birth after previous cesarean delivery. Number 5, July 1999 (replaces practice bulletin number 2, October 1998). Clinical management guidelines for obstetrician-gynecologists. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet . 1999 Aug. 66(2):197-204. [QxMD MEDLINE Link] .
American College of Obstetricians and Gynecologists (ACOG). Vaginal birth after previous cesarean delivery. Washington (DC): American College of Obstetricians and Gynecologists (ACOG); 2010 Aug. 14 p. (ACOG practice bulletin; no. 115).
National Guideline Clearinghouse (NGC). Guideline summary: Vaginal birth after previous cesarean delivery. In: National Guideline Clearinghouse (NGC) Rockville (MD): [cited Feb 16, 2011. [Full Text] .
Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 184: Vaginal Birth After Cesarean Delivery. Obstet Gynecol . 2017 Nov. 130 (5):e217-e233. [QxMD MEDLINE Link] .
Hill JB, Ammons A, Chauhan SP. Vaginal birth after cesarean delivery: comparison of ACOG practice bulletin with other national guidelines. Clin Obstet Gynecol . 2012 Dec. 55(4):969-77. [QxMD MEDLINE Link] .
Grobman WA, Sandoval G, Rice MM, et al. Prediction of vaginal birth after cesarean delivery in term gestations: a calculator without race and ethnicity. Am J Obstet Gynecol . 2021 Dec. 225 (6):664.e1-664.e7. [QxMD MEDLINE Link] . [Full Text] .
Kaimal AJ, Caughey AB, Gandhi M, et al. Counseling Regarding Approach to Delivery After Cesarean and the Use of a Vaginal Birth After Cesarean Calculator. American College of Obstetricians and Gynecologists. Available at https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2021/12/counseling-regarding-approach-to-delivery-after-cesarean-and-the-use-of-a-vaginal-birth-after-cesarean-calculator . December 2021; Accessed: June 9, 2023.
Rosen MG, Dickinson JC, Westhoff CL. Vaginal birth after cesarean: a meta-analysis of morbidity and mortality. Obstet Gynecol . 1991 Mar. 77(3):465-70. [QxMD MEDLINE Link] .
Flamm BL, Geiger AM. Vaginal birth after cesarean delivery: an admission scoring system. Obstet Gynecol . 1997 Dec. 90(6):907-10. [QxMD MEDLINE Link] .
Quiñones JN, Stamilio DM, Paré E, Peipert JF, Stevens E, Macones GA. The effect of prematurity on vaginal birth after cesarean delivery: success and maternal morbidity. Obstet Gynecol . 2005 Mar. 105(3):519-24. [QxMD MEDLINE Link] .
Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med . 2004 Dec 16. 351(25):2581-9. [QxMD MEDLINE Link] .
Miller DA, Diaz FG, Paul RH. Vaginal birth after cesarean: a 10-year experience. Obstet Gynecol . 1994 Aug. 84(2):255-8. [QxMD MEDLINE Link] .
Flamm BL, Goings JR, Liu Y, Wolde-Tsadik G. Elective repeat cesarean delivery versus trial of labor: a prospective multicenter study. Obstet Gynecol . 1994 Jun. 83(6):927-32. [QxMD MEDLINE Link] .
McMahon MJ, Luther ER, Bowes WA Jr, Olshan AF. Comparison of a trial of labor with an elective second cesarean section. N Engl J Med . 1996 Sep 5. 335(10):689-95. [QxMD MEDLINE Link] .
Shipp TD, Zelop CM, Repke JT, Cohen A, Caughey AB, Lieberman E. Intrapartum uterine rupture and dehiscence in patients with prior lower uterine segment vertical and transverse incisions. Obstet Gynecol . 1999 Nov. 94(5 Pt 1):735-40. [QxMD MEDLINE Link] .
Macones GA, Peipert J, Nelson DB, Odibo A, Stevens EJ, Stamilio DM, et al. Maternal complications with vaginal birth after cesarean delivery: a multicenter study. Am J Obstet Gynecol . 2005 Nov. 193(5):1656-62. [QxMD MEDLINE Link] .
Leung AS, Farmer RM, Leung EK, Medearis AL, Paul RH. Risk factors associated with uterine rupture during trial of labor after cesarean delivery: a case-control study. Am J Obstet Gynecol . 1993 May. 168(5):1358-63. [QxMD MEDLINE Link] .
Zelop CM, Shipp TD, Repke JT, Cohen A, Lieberman E. Effect of previous vaginal delivery on the risk of uterine rupture during a subsequent trial of labor. Am J Obstet Gynecol . 2000 Nov. 183(5):1184-6. [QxMD MEDLINE Link] .
Zelop CM, Shipp TD, Repke JT, Cohen A, Caughey AB, Lieberman E. Uterine rupture during induced or augmented labor in gravid women with one prior cesarean delivery. Am J Obstet Gynecol . 1999 Oct. 181(4):882-6. [QxMD MEDLINE Link] .
Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med . 2001 Jul 5. 345(1):3-8. [QxMD MEDLINE Link] .
Wing DA, Lovett K, Paul RH. Disruption of prior uterine incision following misoprostol for labor induction in women with previous cesarean delivery. Obstet Gynecol . 1998 May. 91(5 Pt 2):828-30. [QxMD MEDLINE Link] .
Cahill A, Stamilio DM, Paré E, Peipert JP, Stevens EJ, Nelson DB, et al. Vaginal birth after cesarean (VBAC) attempt in twin pregnancies: is it safe?. Am J Obstet Gynecol . 2005 Sep. 193(3 Pt 2):1050-5. [QxMD MEDLINE Link] .
Miller DA, Mullin P, Hou D, Paul RH. Vaginal birth after cesarean section in twin gestation. Am J Obstet Gynecol . 1996 Jul. 175(1):194-8. [QxMD MEDLINE Link] .
Delaney T, Young DC. Trial of labour compared to elective Caesarean in twin gestations with a previous Caesarean delivery. J Obstet Gynaecol Can . 2003 Apr. 25(4):289-92. [QxMD MEDLINE Link] .
Strong TH Jr, Phelan JP, Ahn MO, Sarno AP Jr. Vaginal birth after cesarean delivery in the twin gestation. Am J Obstet Gynecol . 1989 Jul. 161(1):29-32. [QxMD MEDLINE Link] .
Ravasia DJ, Brain PH, Pollard JK. Incidence of uterine rupture among women with müllerian duct anomalies who attempt vaginal birth after cesarean delivery. Am J Obstet Gynecol . 1999 Oct. 181(4):877-81. [QxMD MEDLINE Link] .
Kayem G, Combaud V, Lorthe E, et al. Mortality and morbidity in early preterm breech singletons: impact of a policy of planned vaginal delivery. Eur J Obstet Gynecol Reprod Biol . 2015 Sep. 192:61-5. [QxMD MEDLINE Link] .
Mone F, Harrity C, Mackie A, et al. Vaginal birth after caesarean section prediction models: a UK comparative observational study. Eur J Obstet Gynecol Reprod Biol . 2015 Oct. 193:136-9. [QxMD MEDLINE Link] .
- Vaginal birth after cesarean delivery rates.
- Table 1. Predictors of VBAC Success or Failure
- Table 2: Predictors of Uterine Rupture
- Table 3: Rates of Uterine Rupture
|
|
Prior vaginal delivery | Maternal obesity |
Prior VBAC | Short maternal stature |
Spontaneous labor | Macrosomia |
Favorable cervix | Increased maternal age (>40 y) |
Nonrecurring indication (breech presentation, placenta previa, herpes) | Induction of labor |
Preterm delivery | Recurring indication (cephalopelvic disproportion, failed second stage) |
| Increased interpregnancy weight gain |
| Latina or African American race/ethnicity |
| Gestational age ≥41 wk |
| Preconceptional or gestational diabetes mellitus |
|
|
Classic hysterotomy | Spontaneous labor |
Two or more cesarean deliveries | Prior vaginal delivery |
Single-layer closure | Longer interpregnancy interval |
Induction of labor | Preterm delivery |
Use of prostaglandins |
|
Short interpregnancy interval |
|
Infection at prior cesarean delivery |
|
|
|
| |
Miller (1994) | 10,880 | 63 (0.6%)* | |
Flamm (1994) | 5,022 | 39 (0.8%) | |
McMahon (1996) | 3,249 | 10 (0.3%) | |
Shipp (1999) | 2,912 | 28 (1%) | |
Landon (2004) | 17,898 | 124 (0.7 %) | |
Macones (2005) | 13,331 | 128 (0.9%) | |
*Includes unknown | |||
Contributor Information and Disclosures
Aaron B Caughey, MD, MPH, PhD Department Chair, Department of Obstetrics and Gynecology, Julie Newpert Stott Director of Center for Women's Health, Oregon Health and Science University School of Medicine Aaron B Caughey, MD, MPH, PhD is a member of the following medical societies: American College of Obstetricians and Gynecologists , Society for Maternal-Fetal Medicine , Society for Medical Decision Making , Society for Reproductive Investigation Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Received salary from Medscape for employment. for: Medscape.
Carl V Smith, MD The Distinguished Chris J and Marie A Olson Chair of Obstetrics and Gynecology, Professor, Department of Obstetrics and Gynecology, Senior Associate Dean for Clinical Affairs, University of Nebraska Medical Center Carl V Smith, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Association of Professors of Gynecology and Obstetrics , Central Association of Obstetricians and Gynecologists , Society for Maternal-Fetal Medicine , Council of University Chairs of Obstetrics and Gynecology , Nebraska Medical Association Disclosure: Nothing to disclose.
Steven David Spandorfer, MD Assistant Professor, Department of Obstetrics and Gynecology, New York Presbyterian Hospital, Weill Cornell Medical College Steven David Spandorfer, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Society for Reproductive Medicine , Endocrine Society Disclosure: Nothing to disclose.
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- HIV in Pregnancy
- Pulmonary Disease and Pregnancy
- Kidney Disease and Pregnancy
- Vaccinations/Immunizations During Pregnancy
- Common Pregnancy Complaints and Questions
- Cardiovascular Disease and Pregnancy
- Multifetal Pregnancy
- Is immunotherapy for cancer safe in pregnancy?
- Labetalol, Nifedipine: Outcome on Pregnancy Hypertension
- Are Nicotine Patches and E-Cigarettes Safe in Pregnancy?

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 2020/viewarticle/immunotherapy-cancer-safe-pregnancy-2024a100083dnews news Is immunotherapy for cancer safe in pregnancy?

- 2002261369-overviewDiseases & Conditions Diseases & Conditions Postterm Pregnancy

The Impact of a VBAC on the 3rd birth*
Nov 09, 2014
10 likes | 96 Views
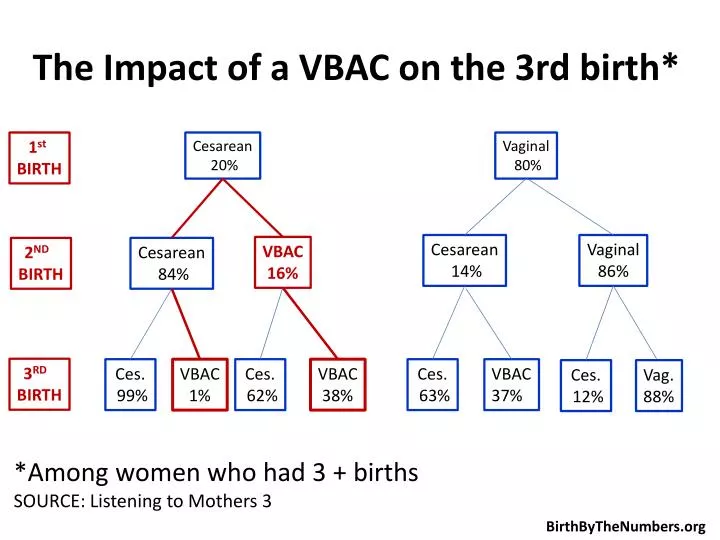
The Impact of a VBAC on the 3rd birth*. Cesarean 2 0%. 1 st BIRTH. Vaginal 80%. Cesarean 14%. Vaginal 86%. VBAC 16%. Cesarean 84%. 2 ND BIRTH. 3 RD BIRTH. Ces. 99%. VBAC 1 %. Ces. 62%. VBAC 38%. VBAC 37%. Ces. 63%. Ces. 12%. Vag. 88%.
Share Presentation
- source listening

Presentation Transcript
The Impact of a VBAC on the 3rd birth* Cesarean 20% 1st BIRTH Vaginal 80% Cesarean 14% Vaginal 86% VBAC 16% Cesarean 84% 2ND BIRTH 3RD BIRTH Ces. 99% VBAC 1% Ces. 62% VBAC 38% VBAC 37% Ces. 63% Ces. 12% Vag. 88% *Among women who had 3 + births SOURCE: Listening to Mothers 3 BirthByTheNumbers.org
- More by User

Chapter 4 Prenatal Development and Birth
Chapter 4 Prenatal Development and Birth. Germinal: The First 14 Days Implantation occurs about a week after conception, the burrowing of the organism into the lining of the uterus, where it can be nourished and protected during growth.
1.33k views • 15 slides
Chapter 6: Birth Control
Chapter 6: Birth Control. For use with Human Sexuality Today (4 th Ed.) Bruce King Slides prepared by: Traci Craig. Chapter Overview. Teen Pregnancy in the US Worldwide need for contraception Myths and Ineffective Methods Fertility Awareness Methods Barrier Methods IUD Hormonal Methods
1.3k views • 53 slides
The Birth Pains of the Messiah
The Birth Pains of the Messiah. Have They Started Yet? Robert C. Newman.
1.33k views • 52 slides
ImPACT Concussion Testing
ImPACT Concussion Testing . All WWE Talent with an active booking contract have been given a baseline ImPACT test. An ImPACT test measures the effects of a concussion through cognitive tests. Baseline ImPACT tests are mandatory for all prospective talent during pre-contract screening.
970 views • 1 slides
Examination of the newborn baby
Examination of the newborn baby. Examination at birth. Aim To describe and carry out an examination of a baby soon after birth Objectives To screen for malformations To observe smooth transition to extra uterine life An asses overall of baby ’ s condition. 2.
1.38k views • 44 slides
Repairs for RPD
Repairs for RPD. Repairs and additions to RPD. Occasionally needed. How to avoid?? C areful diagnosis , treatment planning , adequate mouth preparations , and the carrying out of an effective partial denture design with all component parts properly fabricated .
1.63k views • 18 slides
Basic Embryology
Basic Embryology. Embryology. Definition: the study of the origin and development of an organism Prenatal period: before birth 38 weeks from conception to birth (average) “fetal” age Gynecologic timing has been from LMP therefore refers to 40 weeks “gestational” age
1.99k views • 28 slides
From impact factor to influence?
From impact factor to influence?. Kamran Abbasi Acting editor, BMJ. What I will talk about. What is impact factor? What is wrong with impact factor? What are the alternatives? What is influence? What does all this mean?. Citation rates.
2.08k views • 55 slides
Birth Order:
Birth Order:. How Your Family Birth Order Determines Your Kitchen Personality Type. Why is it Important to Understand the Characteristics of Family Birth Order?. Better understanding of interpersonal relationships (you’ll get along better) Better communication
1.34k views • 38 slides
Contraceptives and Birth Control
Contraceptives and Birth Control. LCHS Mark Ewoldsen, Ph.D. Remember. The total risks of birth control are much less than the total risks of a pregnancy. Current US Pattern - 1990. Family size - 2.2 children Reproductive years 17-47 (30) yrs 5-6 methods over life span
1.4k views • 105 slides
CHAPTER 4 PRENATAL DEVELOPMENT AND BIRTH
CHAPTER 4 PRENATAL DEVELOPMENT AND BIRTH. Learning Objectives. How does development unfold during the prenatal period from conception until the time of birth? How does prenatal behavior of the fetus relate to postnatal behavior of the infant?. Prenatal Development.
878 views • 28 slides

Adoptive and Birth Families
Adoptive and Birth Families . Before we begin today . . . . What adoption issues arose for you in your practice since our last class?. Our Learning Objectives: You will be able to . . . . Describe two types of adoptive families and give at least three examples of each.
1.48k views • 129 slides
Birth data quality
Birth data quality. VITAL RECORDS: A CULTURE OF QUALITY NAPHSIS Annual Meeting | Seattle | June 8-11, 2014. the birth data quality workgroup . An Update. Birth Data quality workgroup Hospital reports/ engaging hospitals Subgroup. Karyn Backus (Chair) (CT) Colleen Fontana (Chair) (RI)
1.17k views • 99 slides
Cesarean Birth
Cesarean Birth. Author: Daren Sachet, RNC, BSN, MPA. Cesarean Birth Objectives. Discuss the implications for cesarean birth List the components of providing a safe surgical environment Describe potential complications related to cesarean birth. Indications. Previous Uterine Scar
1.52k views • 86 slides
Birth control and women's empowerment
Birth control and women's empowerment. Pierre Andre Chiappori Sonia Oreffice Conference: The economics of the family London, September 2006. Introduction: Abortion and ‘Female Empowerment ’. General view: abortion as ‘empowering’ women
1.1k views • 82 slides
General Embryology 3
General Embryology 3. Lei Lei Aug.29, 2006. Today’s contents. 3rd month to birth: Fetal membrane and placenta Birth defects and prenatal diagnosis. Chapter 6. Third month to birth: the fetus and placenta. Ⅰ. Development of the fetus Ⅱ. Fetal membranes: Chorion Ⅲ. Placenta ★.
1.12k views • 61 slides
BIRTH ORDER From ADLER To SULLOWAY
BIRTH ORDER From ADLER To SULLOWAY. A 32-year Review of Literature With A Biopsychosocial Approach. Methodological Standpoints in Birth Order Studies. Between-Family Studies:. Birth Order As A Dependent Variable
1.06k views • 20 slides
Pediatric Nutrition
Pediatric Nutrition. Gestational Age and Size. Low birth weight (LBW) – an infant who weighs less than 2500 g at birth Very low birth weight (VLBW) – an infant who weighs less than 1500 g at birth Extremely low birth weight (ELBW) – an infant weighing less than 1000 g at birth
1.36k views • 61 slides

Unit 3: Birth of Modern America
Unit 3: Birth of Modern America. Chapter 9. Industrialization. I. Introduction to Industrialization. Industrial Revolution 1. Definition: the movement from small-scale manufacturing to the production of heavy industry, using machines to replace human laborers
1.08k views • 87 slides
Nicholas Sparks
Nicholas Sparks. Important Facts about Sparks. Date of birth: December 31, 1965 Place of birth: Omaha, Nebraska
1.18k views • 9 slides
Is Jesus God? What the bible says? (v .1)
Is Jesus God? What the bible says? (v .1). Supernatural Birth. Mat 1:18 Now the birth of Jesus Christ happened in this way. When his mother Mary was engaged to Joseph, before they lived together she was discovered to be pregnant by the Holy Spirit. He is `God with us’. Prophecy in 700 BC
1.37k views • 88 slides

For Physicians. By Physicians.™
- My ObGFirst Account
- Edit Billing Info
- Edit Profile info
- 2T US Atlas
- Evidence Matters
- Primary Care
- Your Practice
- My Bookshelf
VBAC Guidelines: Who is a Candidate for a Trial of Labor after Cesarean Delivery?

While trial of labor after cesarean delivery (TOLAC) may be considered after previous cesarean delivery, it is critical that a thorough review of risks and benefits be undertaken. Decision making should incorporate a woman’s preferences and desires. Key highlights from the most recent ACOG guidance include the following:
CLINICAL ACTIONS:
Candidates for tolac (level a).
- Singleton: One previous low transverse cesarean should be counseled and offered TOLAC
- Even if patient not a good candidate but admitted to labor floor in active labor, clinical judgement may be used
- Good candidates are those where balance of risk (low) and chance of success (high) are acceptable to patient and provider
- Decisions surrounding TOLAC should include discussion of future pregnancies
NOT Candidates for TOLAC (Level B)
- Previous classical or “T” incision
- ACOG states
“…similar to a history of a prior classical cesarean, the suggested timing of delivery between 36 0/7 weeks and 37 0/7 weeks of gestation should be considered but can be individualized based on the clinical situation”
- Extensive transfundal uterine surgery
- Contraindication for vaginal delivery (e.g. placenta previa)
More than One Previous Cesarean Section (Level B)
- Two previous low transverse cesarean should be counseled and offered TOLAC
- Data limited on >2 previous cesarean sections
Macrosomia (birth weight >4,000 g or 4,500 g)
- Less likelihood of VBAC but data on rupture inconclusive
- Isolated macrosomia does ‘not preclude’ TOLAC
Gestational Age > 40 Weeks
- Less likelihood of VBAC but data on rupture conflicting
- Gestational age > 40 alone does ‘not preclude’ TOLAC
Previous (documented) Low-Vertical incision (Level B)
- The few studies on this topic demonstrate similar rate of VBAC success and no consistent evidence of rupture/morbidities
- Consider limited data but provider and patient may elect TOLAC
Unknown Prior Uterine Incision (Level B)
- Previous case series reported VBAC success and rupture rates similar to known low transverse scars
- Women with one previous cesarean, unknown scar, may be candidates for TOLAC if no clinical suspicion for classical incision is apparent (e.g., early preterm)
Twin Gestation
- Consistent evidence that outcomes are similar to singletons
- Women with twin gestation and one previous low transverse scar cesarean section are candidates for TOLAC
- BMI alone is not an absolute contraindication but should be considered an additional risk factor that may lower chance of VBAC
- Obese women have increased risk related to cesarean section
- Individualize care
Induction and Augmentation of Labor
- Induction of labor an option (Level B)
- While data does support a dose/response relationship between oxytocin use and rupture, no threshold has been identified and therefore “an upper limit for oxytocin dosage with TOLAC has not been established”
- 1.4% risk of rupture for prostaglandins +/- oxytocin
- 1.1% oxytocin alone
- 0.9% augmented labor
- 0.4% spontaneous labor (expectant management and not spontaneous labor is the preferable control group and not available in this study)
- Increased risk only in women without a prior vaginal delivery
- Favorability of cervix unrelated to outcome
- Dose-response with oxytocin use but no clear threshold for rupture
While there are risks to TOLAC, most are related to complications, such as hemorrhage, that may arise from cesarean section in the setting of an unsuccessful trial of labor. However, TOLAC is still offered to patients as an option due to the significant risks associated with multiple repeat cesarean deliveries. Risks of placenta accreta, cystotomy, bowel injury, ureteral injury, and ileus, the need for postoperative ventilation, intensive care unit admission, hysterectomy, and blood transfusion requiring 4 or more units, and the duration of operative time and hospital stay significantly increase with increasing number of cesarean deliveries. In the NICHD MFMU study (Obstetrics and Gynecology 2006), Placenta accreta was present in 0.24% (1st cesarean sections [CS]) 0.31% (2nd CS), 0.57% (3rd CS), 2.13% (4th CS), 2.33% (5th CS), 6.74% (6 or more CS). Hysterectomy was required in 0.65% (1st CS) 0.42% (2nd CS) (0.90% (3rd CS) 2.41% (4th CS) 3.49% (5th CS) and 8.99% (6 or more CS). In 723 women who had previa in this study, risk for placenta accreta was 3% (1st CS), 11% (2nd CS), 40% (3rd CS) 61% (4th CS), and 67% (5 or more CS).
KEY POINTS:
Clinical Factors and Probability of Success
- Prior vaginal delivery
- Spontaneous labor
- Labor dystocia as the indication for primary cesarean section
- Increased maternal age
- Non-white ethnicity
- Gestational age greater than 40 weeks
- Maternal obesity
- Preeclampsia
- Short inter-pregnancy interval
- Increased neonatal birthweight
- The MFMU Network VBAC calculator has been updated and no longer includes race or ethnicity | The calculator can be found in ‘Learn More – Primary Sources’
- Data derived from Grobman et al. (AJOG, 2021)
- The calculator should not be used as the only measure for determining patient management
Note: ACOG addresses the use of VBAC calculators and stresses the importance of shared decision making, highlighting the point that a VBAC calculator is just one aspect of the discussion
Currently, there is no evidence demonstrating improved patient outcomes and therefore
A VBAC calculator score should not be used as a barrier to TOLAC …some patients and clinicians may prefer to utilize a calculator while others may prefer a more general discussion of options for mode of delivery, review of overall VBAC rates of 60–80% with TOLAC, and consideration of an individual’s obstetric risk factors along with their preferences and goals
CLINICAL CONSIDERATIONS:
- Mechanical dilation and transcervical catheters may be an option
- Misoprostol should not be used in pregnancies at term for cervical ripening or labor induction in patients who have had a cesarean delivery or major uterine surgery (Level A)
- Prostaglandins can be considered during 2nd trimester
- Insufficient evidence to make a definitive recommendation for prostaglandin E2
- External cephalic version for breech presentation is not contraindicated in women with a prior low transverse uterine scar (Level B)
- Epidural analgesia for labor may be used as part of TOLAC (Level A)| Not considered necessary
- Use similar standards to gauge progress of labor
- The decision to undergo TOLAC or repeat cesarean section, following counseling, should be made by the patient in consultation with her providers
- Evidence lacking that IUPC or fetal scalp electrodes are better than external forms of continuous monitoring
- IUPC may not help diagnose uterine rupture
- Include the potential risks and benefits of both TOLAC and elective repeat cesarean section
- Management plan
Additional Highlights from the Canadian Evidence Review and Guidelines (2019)
- Baseline risk with TOLAC is 0.47%
- With induction (not contraindicated), risk of rupture highest >40 weeks gestation
- Prostaglandin E2 not recommended due to increased risk of rupture
- “Is necessary” because changes in the tracing are “one of the key indicators of the presence of a uterine rupture”
- Not an absolute contraindication
- Advise that there is insufficient information to assess TOLAC risks
- There is relationship between lower uterine thickness and risk of uterine rupture
- Absolute cut-offs not known at this time
- Ultrasonographic measurements of the lower uterine segment can not be used to counsel regarding TOLAC
- Women should be made aware that their is an increased risk of uterine rupture with single vs double uterine closure
Learn More – Primary Sources:
ACOG Practice Bulletin 205: Vaginal birth after previous cesarean delivery
Maternal morbidity associated with multiple repeat cesarean deliveries
MFMU Network Calculator for VBAC
ACOG Practice Advisory: Counseling Regarding Approach to Delivery After Cesarean and the Use of a Vaginal Birth After Cesarean Calculator
Prediction of vaginal birth after cesarean in term gestations: A calculator without race and ethnicity
Want to be notified when new guidelines are released? Get ObGFirst!
Related obg topics:.

- Sexual Health
- Cervical Health Resource Center
Are you an ObG Insider?
Get specially curated clinical summaries delivered to your inbox every week for free
Subscribe to ObG
Already an ObGFirst Member? Welcome back
Want to sign up? Get guideline notifications CME Included
Sign Up for ObGFirst and Stay Ahead
- - Professional guideline notifications
- - Daily summary of a clinically relevant research paper
- - Includes 1 hour of CME every month
Already a Member of ObGFirst ® ?
Please log in to ObGFirst to access this page
Not an ObGFirst ® Member Yet?
- - Access 2T US Atlas
- - Guideline notifications
- - Daily research paper summaries
- - And lots more!

Media - Internet
Computer system requirements.
OBG Project CME requires a modern web browser (Internet Explorer 10+, Mozilla Firefox, Apple Safari, Google Chrome, Microsoft Edge). Certain educational activities may require additional software to view multimedia, presentation, or printable versions of their content. These activities will be marked as such and will provide links to the required software. That software may be: Adobe Flash, Apple QuickTime, Adobe Acrobat, Microsoft PowerPoint, Windows Media Player, or Real Networks Real One Player.
Disclosure of Unlabeled Use
This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the FDA. The planners of this activity do not recommend the use of any agent outside of the labeled indications.
The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the planners. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications, and warnings.
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s conditions and possible contraindications and/or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
Jointly provided by

NOT ENOUGH CME HOURS
It appears you don't have enough CME Hours to take this Post-Test. Feel free to buy additional CME hours or upgrade your current CME subscription plan
Leaving ObG Website
You are now leaving the ObG website and on your way to PRIORITY at UCSF, an independent website. Therefore, we are not responsible for the content or availability of this site
- Screening & Prevention
- Sexual Health & Relationships
- Birth Control
- Preparing for Surgery Checklist
- Healthy Teens
- Getting Pregnant
- During Pregnancy
- Labor and Delivery
- After Pregnancy
- Pregnancy Book
- Mental Health
- Prenatal Testing
- Menstrual Health
- Heart Health
- Special Procedures
- Diseases and Conditions
- Browse All Topics
- View All Frequently Asked Questions

Read common questions on the coronavirus and ACOG’s evidence-based answers.
Vaginal Birth After Cesarean Delivery (VBAC)
URL has been copied to the clipboard
Frequently Asked Questions Expand All
If you have had a previous cesarean delivery, you have two choices about how to give birth again:
You can have a scheduled cesarean delivery.
You can give birth vaginally. This is called a VBAC.
A TOLAC is the attempt to have a VBAC. If it is successful, TOLAC results in a vaginal birth. If it is not successful, you will need another cesarean delivery.
A successful VBAC has the following benefits:
No abdominal surgery
Shorter recovery period
Lower risk of infection
Less blood loss
Many women would like to have the experience of vaginal birth, and when successful, VBAC allows this to happen. For women planning to have more children, VBAC may help them avoid certain health problems linked to multiple cesarean deliveries. These problems can include bowel or bladder injury, hysterectomy , and problems with the placenta in future pregnancies. If you know that you want more children, this may figure into your decision.
Some risks of a VBAC are infection, blood loss, and other complications. One rare but serious risk with VBAC is that the cesarean scar on the uterus may rupture (break open). Although a rupture of the uterus is rare, it is very serious and may harm both you and your fetus . If you are at high risk of rupture of the uterus, VBAC should not be tried.
After cesarean delivery, you will have a scar on your skin and a scar on your uterus. Some uterine scars are more likely than others to cause a rupture during VBAC. The type of scar depends on the type of cut in the uterus:
Low transverse—A side-to-side cut made across the lower, thinner part of the uterus. This is the most common type of incision and carries the least chance of future rupture.
Low vertical—An up-and-down cut made in the lower, thinner part of the uterus. This type of incision carries a higher risk of rupture than a low transverse incision.
High vertical (also called “classical”)—An up-and-down cut made in the upper part of the uterus. This is sometimes done for very preterm cesarean deliveries. It has the highest risk of rupture.
You cannot tell what kind of cut was made in the uterus by looking at the scar on the skin. Medical records from the previous delivery should include this information. It is a good idea to get your medical records of your prior cesarean delivery so your obstetrician-gynecologist (ob-gyn) or other health care professional can review them.
VBAC should take place in a hospital that can manage situations that threaten the life of the woman or her fetus. Some hospitals may not offer VBAC because hospital staff do not feel they can provide this type of emergency care. You and your ob-gyn or other health care professional should consider the resources available at the hospital you have chosen.
If you have chosen to try a VBAC, things can happen that alter the balance of risks and benefits. For example, you may need to have your labor induced (started with drugs or other methods). This can reduce the chances of a successful vaginal delivery. Labor induction also may increase the chance of complications during labor. If circumstances change, you and your ob-gyn or other health care professional may want to reconsider your decision.
The reverse also may be true. For example, if you have planned a cesarean delivery but go into labor before your scheduled surgery, it may be best to consider VBAC if you are far enough along in your labor and your fetus is healthy.
Cesarean Delivery : Delivery of a baby through surgical incisions made in the woman’s abdomen and uterus.
Fetus : The stage of prenatal development that starts 8 weeks after fertilization and lasts until the end of pregnancy.
Hysterectomy : Removal of the uterus.
Obstetrician–Gynecologist (Ob-Gyn) : A physician who specializes in caring for women during pregnancy, labor, and the postpartum period.
Placenta : Tissue that provides nourishment to and takes waste away from the fetus.
Uterus : A muscular organ located in the female pelvis that contains and nourishes the developing fetus during pregnancy.
Article continues below
Advertisement
If you have further questions, contact your ob-gyn.
Don't have an ob-gyn? Learn how to find a doctor near you .
Published: December 2017
Last reviewed: August 2022
Copyright 2024 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information . This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer .
Clinicians: Subscribe to Digital Pamphlets
Explore ACOG's library of patient education pamphlets.
A Guide to Pregnancy from Ob-Gyns
For trusted, in-depth advice from ob-gyns, turn to Your Pregnancy and Childbirth: Month to Month.
ACOG Explains
A quick and easy way to learn more about your health.
What to Read Next
Finding Support in the Postpartum Period
An Ob-Gyn's Guide to Standing Up for Yourself During Pregnancy
Cesarean Birth
Postpartum Pain Management
Appointments at Mayo Clinic
- Labor and delivery, postpartum care
VBAC: Know the pros and cons
Wonder if you're a good candidate for VBAC? If the benefits of VBAC outweigh the risks? The answer might be up to you. Here's help weighing the pros and cons.
Many women are candidates for vaginal birth after cesarean (VBAC). In 2013, the success rate for women in the U.S. who attempted a trial of labor (TOLAC) after one previous cesarean was 70%.
Still, the choice to pursue VBAC or schedule a repeat C-section can be difficult. Here's insight on how to make the decision.
Why consider VBAC?
Compared with having another C-section, a vaginal delivery involves no surgery, none of the possible complications of surgery, a shorter hospital stay and a quicker return to normal daily activities. VBAC might also be appealing if you want to experience vaginal childbirth.
It's important to consider future pregnancies, too. If you're planning for more pregnancies, VBAC might help you avoid the risks of multiple cesarean deliveries, such as placental problems.
What are the risks of VBAC?
While a successful VBAC is associated with fewer complications than an elective repeat C-section, a failed trial of labor after a C-section is associated with more complications, including a uterine rupture. Uterine rupture is rare, happening in less than 1% of women who attempt a trial of labor after cesarean. However, uterine rupture is life-threatening for you and your baby. During a uterine rupture, the cesarean scar on the uterus breaks open. An emergency C-section is needed to prevent life-threatening complications. Treatment might involve surgical removal of the uterus (hysterectomy). If your uterus is removed, you won't be able to get pregnant again.
Who's eligible for VBAC?
VBAC eligibility depends on many factors. For example:
- What type of uterine incision was used for the prior C-section? Most C-sections use a low transverse incision. Women who have had a low transverse or low vertical incision are usually VBAC candidates. If you've had a prior high vertical (classical) incision, VBAC isn't recommended because of the risk of uterine rupture.
- Have you ever had a uterine rupture? If so, you're not a candidate for VBAC .
- Have you had other surgeries on your uterus? If you've had other uterine surgeries, such as for fibroid removal, VBAC isn't recommended due to the risk of uterine rupture.
- Have you had previous vaginal deliveries? A vaginal delivery at least once before or after your prior C-section increases the probability of a successful VBAC .
- How many C-sections have you had? Many health care providers won't offer VBAC if you've had more than two prior C-sections.
- When did you last give birth? The risk of uterine rupture is higher if you attempt VBAC less than 18 months after your previous delivery.
- Do you have any health concerns that might affect a vaginal delivery? A C-section might be recommended if you have placental problems, your baby is in an abnormal position, or you're carrying triplets or higher order multiples.
- Where will you deliver the baby? Plan to deliver at a facility equipped to handle an emergency C-section. A home delivery isn't appropriate for VBAC .
- Will you need to be induced? Having labor induced decreases the likelihood of a successful VBAC .
How does labor and delivery during VBAC differ from labor and delivery during a routine vaginal birth?
If you choose VBAC , when you go into labor you'll follow a process similar to that used for any vaginal delivery. However, your health care provider will likely recommend continuous monitoring of your baby's heart rate and be prepared to do a repeat C-section if needed.
What other advice do you offer women who are considering VBAC?
If you're considering VBAC , discuss the option, your concerns and your expectations with your health care provider early in pregnancy. Make sure he or she has your complete medical history, including records of your previous C-section and any other uterine procedures. Your health care provider might calculate the likelihood that you'll have a successful VBAC .
Also, plan to deliver your baby at a facility that's equipped to handle an emergency C-section. Continue discussing the risks and benefits of VBAC throughout pregnancy, especially if certain risk factors arise.
Above all, try to stay flexible. The circumstances of your labor could make VBAC a clear choice or, after counseling, you and your health care provider might decide that a repeat C-section would be best after all.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Metz TD. Choosing the route of delivery after cesarean birth. https://www.uptodate.com/contents/search. Accessed Feb. 13, 2020.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 205: Vaginal birth after cesarean delivery. Obstetrics & Gynecology. 2019; doi:10.1097/AOG.0000000000003078.
- AskMayoExpert. Vaginal birth after cesarean (VBAC). Mayo Clinic; 2019.
- Frequently asked questions. Labor, delivery and postpartum care FAQ070. Vaginal birth after cesarean delivery. American College of Obstetricians and Gynecologists. https://www.acog.org/Patients/FAQs/Vaginal-Birth-After-Cesarean-Delivery. Accessed Feb. 13, 2020.
- Gabbe SG, et al., eds. Vaginal birth after cesarean delivery. In: Obstetrics: Normal and Problem Pregnancies. 7th ed. Elsevier; 2017. https://www.clinicalkey.com. Accessed Feb. 14, 2020.
- Uterine rupture. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gynecology-and-obstetrics/abnormalities-and-complications-of-labor-and-delivery/uterine-rupture#. Accessed Feb. 14, 2020.
Products and Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Can vaginal tears during childbirth be prevented?
- Fetal presentation before birth
- High-risk pregnancy
- Inducing labor
- Labor pain medications
- Labor positions
- Repeat C-sections
- Signs of labor
- Stages of labor and birth
- Tailbone pain
- Vaginal tears in childbirth
- The epidural block
- Water breaking
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- VBAC Know the pros and cons
Double your impact on fighting cancer
Make a gift before July 31 and it can go twice as far to fight cancer.
Clinical Practice Guideline
Vaginal birth after cesarean, (developed by the aafp, may 2014) (reaffirmed 2019).
The guideline, Labor After Cesarean/Planned Vaginal Birth After Cesarean , was developed by the American Academy of Family Physicians. It was approved by the Board of Directors in 2014 and an executive summary was published in the Annals of Family Medicine on January 12, 2015.
Key Recommendations
- Counseling, encouragement and facilitation for a planned vaginal birth after cesarean (PVBAC) should be provided so that women can make informed decisions. If PVBAC is not locally available, then women desiring it should be offered referral to a facility or clinician who can offer the service.
- Indications for and circumstances surrounding the prior cesarean birth(s) should be discussed.
- Induction of labor after cesarean is appropriate for women who have a medical indication for induction of labor and who are planning a LAC/VBAC. Misoprostol should not be used for cervical preparation or induction of labor in the third trimester of pregnancy for women with a prior cesarean birth.
- At time of labor and presentation to the hospital, the plan for labor and vaginal birth should be reassessed with consideration of factors on admission that may affect the risks of labor and likelihood of vaginal birth. Any changes in status during labor should be discussed.
- Patients should be informed of the specific short-term and long-term benefits and harms of planned LAC/VBAC for the patient, her fetus/infant, and future pregnancies.
- All women desiring planned LAC/VBAC should be counseled about the capabilities of their specific delivery setting and women at high risk for complications should be referred as necessary to facilities with capabilities to effectively treat problems as they develop.
- Hospitals should have guidelines to promote access to LAC/VBAC and actively monitor and improve quality of care for women who choose labor after cesarean.
Read the full recommendation for further details.
More About Practice Guidelines
These recommendations are provided only as assistance for physicians making clinical decisions regarding the care of their patients. As such, they cannot substitute for the individual judgment brought to each clinical situation by the patient's family physician. As with all clinical reference resources, they reflect the best understanding of the science of medicine at the time of publication, but they should be used with the clear understanding that continued research may result in new knowledge and recommendations. These recommendations are only one element in the complex process of improving the health of America. To be effective, the recommendations must be implemented.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Follow. 1) Vaginal birth after cesarean section (VBAC) has been a controversial issue in obstetrics, as opinions have changed over time on whether a scarred uterus can support a vaginal birth. 2) While it was once believed that "once a cesarean, always a cesarean" was necessary, research now shows that 70-80% of women with a prior low ...
VBAC score - admission Bishop score, age, previous caesarean delivery indication, body mass index (BMI) and previous vaginal birth. a VBAC score of more than 16 was greater than 85%, in contrast to those with a VBAC score of 10 who had a 49% success. Women with prior uterine rupture or classical or T-shaped incision ideally should undergo ...
Vaginal birth after cesarean section (VBAC) is the term applied to women who undergo vaginal delivery following cesarean delivery in a prior pregnancy. Patients desiring VBAC delivery undergo a trial of labor (TOL) or trial of labor after cesarean section (TOLAC). Vaginal birth after C-section.
Vaginal birth after caesarean, commonly referred to as VBAC, is a term used to describe the delivery of a baby vaginally by a woman who has had at least one previous caesarean section (C-section). Vaginal birth after caesarean is becoming increasingly popular as more women seek to avoid the potential risks associated with a repeat C-section. VBAC can be a safe and viable option for many women ...
Read terms. ABSTRACT: Trial of labor after cesarean delivery (TOLAC) refers to a planned attempt to deliver vaginally by a woman who has had a previous cesarean delivery, regardless of the outcome. This method provides women who desire a vaginal delivery the possibility of achieving that goal—a vaginal birth after cesarean delivery (VBAC).
Vaginal Birth After C-Section • To reorder Patient Education Pamphlets in packs of 50, please call 800-762-2264 or order online at sales.acog.org. • The American College of Obstetricians and Gynecologists409 12th Street, SWPO Box 96920Washington, DC 20090-6920. Vaginal Birth After Cesarean (VBAC). The Changing Tide. What Are Hospital Policies?.
Although attempts at a trial of labor after a cesarean birth (TOLAC) have become accepted practice, the rate of successful vaginal birth after cesarean delivery (VBAC), as well as the rate of attempted VBACs, decreased during a 10-year period (see the image below). Whereas 40-50% of women attempted VBAC in 1996, as few as 20% of patients with a ...
The Impact of a VBAC on the 3rd birth* An Image/Link below is provided (as is) to download presentation Download Policy: Content on the Website is provided to you AS IS for your information and personal use and may not be sold / licensed / shared on other websites without getting consent from its author.
ppt VBAC - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. This case discusses a 32-33 week preterm parturient with a previous cesarean section who presents in active labor and is COVID-19 positive. After examination and consultation, an emergency c-section was planned.
Vaginal Birth After Cesarean Giving your patient all the facts Objectives We will We will We will VBAC We will VBAC We will who is. ... Study Resources. Log in Join. VBAC presentation.pptx - Vaginal Birth After Cesarean... Doc Preview. Pages 10. Identified Q&As 1. Solutions available. Total views 9. Simmons College. NURS. NURS MISC ...
59 likes • 7,521 views. AI-enhanced description. Alicia Tan. This document provides information on vaginal birth after caesarean (VBAC) including definitions, risks, guidelines and a case study. It defines key terms like VBAC, discusses risks to mother and baby like uterine rupture, and outlines factors that increase unsuccessful VBAC rates.
2314546778905478755 o 5 of 31 52 5377551070685854870 There is a consensus (National Institute for Health and Care Excellence [NICE],6 Royal College of Obstetricians and Gynaecologists [RCOG], 1 American College of Obstetricians and Gynecologists [ACOG]/ National Institutes of Health [NIH]7-9) that planned VBAC is a clinically safe choice for the majority of
presentation) (39-44). Similarly, there is consistent evi-dence that women who undergo labor induction or aug-mentation are less likely to achieve VBAC than women with fetuses of the same gestational age in spontaneous labor without augmentation (45-48). Other factors that negatively influence the likelihood of VBAC include
VBAC - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Madam M, who is 28 weeks pregnant with her second child, had a previous c-section delivery due to breech presentation. She is interested in attempting a vaginal birth after cesarean (VBAC) for her current pregnancy.
Chapter 19 -Page 6 Vaginal Birth After Caesarean Section. Use of prostaglandins followed by oxytocin is contraindicated. Mechanical cervical ripening with a Foley catheter is an option. All of these issues should be carefully considered and discussed with the woman before a management plan is finalized.
Candidates for TOLAC (Level A) Singleton: One previous low transverse cesarean should be counseled and offered TOLAC. Individualize. Even if patient not a good candidate but admitted to labor floor in active labor, clinical judgement may be used. Good candidates are those where balance of risk (low) and chance of success (high) are acceptable ...
Vbacs. This document discusses the history and risks/benefits of vaginal birth after cesarean (VBAC) versus elective repeat cesarean section. It notes that while VBAC was originally encouraged due to risks of multiple c-sections, safety concerns led to declining VBAC rates. VBAC carries risks of uterine rupture but reduces risks of respiratory ...
For trusted, in-depth advice from ob-gyns, turn to Your Pregnancy and Childbirth: Month to Month. Learn About the Book. After a cesarean delivery, you may be able to give birth to your next baby vaginally. VBAC may help avoid certain health problems linked to multiple cesarean deliveries.
While a successful VBAC is associated with fewer complications than an elective repeat C-section, a failed trial of labor after a C-section is associated with more complications, including a uterine rupture. Uterine rupture is rare, happening in less than 1% of women who attempt a trial of labor after cesarean. However, uterine rupture is life-threatening for you and your baby.
Lscs and Vbac. This document discusses caesarean sections and vaginal birth after caesarean (VBAC). It outlines the most common indications for caesarean section including previous c-section, dystocia, fetal distress, and breech presentation. It describes the procedure for a lower segment caesarean section and complications that can occur.
The guideline, Labor After Cesarean/Planned Vaginal Birth After Cesarean, was developed by the American Academy of Family Physicians. It was approved by the Board of Directors in 2014 and an ...
1. DR.PRIYA SAXENA VAGINAL BIRTH AFTER CESAREAN (VBAC) 2. CURRENT RECOMMENDATIONS FOR TOLAC AND VBAC Only one previous low segment transverse cesarean delivery. VBAC can also be allowed in women with previous 2 LSCS with a vaginal delivery after counselling Clinically pelvis should be adequate on clinical examination No other uterine scar (eg ...
For all labours, a meta-analysis showed that epidural analgesia increased the risk of second stage delay and operative instrumental vaginal delivery.117 It is appropriate to consider early placement of the epidural catheter so that it can be used later for labour analgesia or for anaesthesia should an operative delivery become necessary.118 One ...