
10 Root Cause Analysis Examples

Viktoriya Sus (MA)
Viktoriya Sus is an academic writer specializing mainly in economics and business from Ukraine. She holds a Master’s degree in International Business from Lviv National University and has more than 6 years of experience writing for different clients. Viktoriya is passionate about researching the latest trends in economics and business. However, she also loves to explore different topics such as psychology, philosophy, and more.
Learn about our Editorial Process

Chris Drew (PhD)
This article was peer-reviewed and edited by Chris Drew (PhD). The review process on Helpful Professor involves having a PhD level expert fact check, edit, and contribute to articles. Reviewers ensure all content reflects expert academic consensus and is backed up with reference to academic studies. Dr. Drew has published over 20 academic articles in scholarly journals. He is the former editor of the Journal of Learning Development in Higher Education and holds a PhD in Education from ACU.

Root cause analysis (RCA) is a problem-solving approach that helps to uncover the underlying causes of an issue or nonconformance to avoid its reoccurrence.
It’s an organized way of addressing issues and seeking out why they happened, not just what occurred and how.
By pinpointing the root cause of any problem, appropriate corrective actions can be taken to ensure similar problems don’t arise again.
The essential steps involved in RCA include:
- Identifying a difficulty
- Performing the root cause analysis
- Creating restorative measures
- Monitoring and verifying results.
As an example, if there has been a surge in customer grievances about delivery times within a transport business, this could be investigated further through root cause analysis.
This approach may identify communication gaps between dispatch staff and drivers as being at fault – leading them to implement better comms systems/training, thus helping prevent future occurrences from happening too often.
Ultimately, root cause analysis proves its worth by uncovering both the ‘what’ and ‘why’ that lie behind problems in order to reach viable outcomes.
Definition of Root Cause Analysis
Root cause analysis (RCA) is an invaluable systematic approach to identifying the source of issues, faults, or nonconformances and delivering lasting solutions.
It involves investigating what initiated a particular event rather than merely tackling its symptoms – making it suitable for industrial accidents, medical errors, and social/behavioral change communication initiatives (Charles et al., 2016).
According to Attar (2022),
“RCA assumes that it is much more effective to systematically prevent and solve underlying issues rather than just treating ad hic symptoms and putting out figures” (p. 87).
In the science and engineering fields, this method has successfully been used as a troubleshooting tool that eliminates root causes associated with any fault or issue.
Similarly, healthcare investigations related to severe adverse events also benefit from RCA using techniques like cause-mapping and templates designed specifically for such purposes.
As stated by Singh and colleagues (2021),
“…root cause analysis has important implications in helping healthcare organizations study events that resulted in patient harm or undesired clinical outcomes and identify strategies to reduce future error and improve patient care and safety” (p. 5).
At the end of it all – thorough root cause analysis can result in effective strategies to prevent future recurrences while simultaneously improving process performance, quality standards, and safety protocols.
In simpler terms, root cause analysis helps us understand why something happened instead of just finding out what occurred along with how it did.
To go broader, see my article on 45 examples of analysis
10 Examples of Root Cause Analysis
- Manufacturing : A computer parts manufacturer identified that their products were failing rapidly due to an underlying design flaw in one of the microchips. So, RCA was conducted, resulting in the development of a new chip designed to eliminate this problem and prevent its recurrence.
- Healthcare : After a patient experienced an unfortunate fall while inside hospital premises, RCA revealed that they weren’t wearing non-slip socks – leading to policy changes ensuring all patients are now provided with these for added safety measures.
- Education : Low student performance on standardized tests triggered an RCA which discovered teachers were not adequately teaching test material. As such, the said institution implemented additional training and support for improved outcomes going forward.
- Software Development : Customer complaints about the software crashing unexpectedly during use called for investigation via RCA, where it became clear there existed bugs causing them. So company enforced rigorous testing processes before any product release was authorized from then onwards.
- Construction : Delay completion of the project necessitated another round of analysis, revealing critical components had been delivered late – prompting the instigation of stricter procurement process protocols guaranteeing timely delivery every time.
- Retail : A retail store notices that their shelves are frequently out of stock. RCA is conducted to identify the root cause, and it is discovered that the store’s ordering process is inadequate, leading to frequent ordering delays. As a result, the store has implemented a new ordering process to eliminate delays and keep shelves fully stocked.
- Aerospace : An airline experienced engine failures following comprehensive investigations finding defects within designs and manufacturing alike. Thus airline took the initiative to work hand-in-hand with the manufacturer on redesigns eliminating errors altogether.
- Energy : Energy providers faced frequent outages due to equipment maintenance neglect. So, they conducted RCA and implemented extra staff dedicated solely to servicing gear, and enacted stringent compliance regulations.
- Finance : Financial institutions’ loss of customers market correlated with negative customer service record. So, remedial action entailed better personnel coaching aiming to enhance satisfaction standards.
- Food Service : A restaurant experiences frequent food safety issues. RCA is conducted to identify the root cause, and it is discovered that employees are not adequately trained in food safety procedures. As a result, the restaurant implements additional training and oversight to ensure compliance with food safety regulations and prevent future issues.
Approaches to Root Cause Analysis
The most common approaches to Root Cause Analysis include the Five Whys, Fishbone Diagrams, Fault Tree Analysis (FTA), Root Cause Mapping, and Pareto Analysis.
Let’s have a look at each of these approaches:
1. Five Whys
The first and the most popular technique in RCA is the Five Whys approach. This simple method involves asking “why” five times until the underlying cause of a problem is revealed (Serrat, 2017).
To illustrate, if a manufacturing company has high product defects, then through a 5 ‘whys’ analysis, it might be determined that there’s no budget allocated because management didn’t make one.
2. Fishbone Diagrams
Alternatively, Fishbone Diagrams or Ishikawa diagrams can identify leading causes by breaking them down into categories or sub-causes (Shinde et al., 2018).
So, in cases where customer satisfaction at restaurants is low due to service quality, food quality, atmosphere, location, and so on being taken into account.
These subbranches are later used to analyze the main reason for customer dissatisfaction.
3. Fault Tree Analysis (FTA)
Fault Tree Analysis (FTA), meanwhile, provides an even more complex route that uses graphical data points representing different possible sources behind problems (Boryczko et al., 2022).
Suppose that an oil rig explodes. So, the FTA would identify all the possible causes, such as equipment failure, human error, procedural problems, environmental factors, etc.
4. Root Cause Mapping
Root Cause Mapping takes a visual tool-based path using human factors, equipment-related issues, process-connected ones, and environmental aspects when analyzing multi-faceted situations (Vanden et al., 2014).
So, if a psychologist analyzes the reason for a child’s depression, they may take into account not only current challenges in their lives but also early childhood, explore how their parents behave, their habits, etc.
5. Pareto Analysis
Last but not least, Pareto Analysis is a statistical technique that quantifies 20% of certain factors accounting for 80% of all mistakes and problems (Vanden et al., 2014).
It makes the decision-making process quite simple by prioritizing what requires improvement first.
Let’s take a restaurant for example: if it experiences constant customer complaints, Pareto analysis may reveal that only a few menu items are responsible for most of them.
Four Steps of Root Cause Analysis
Root cause analysis (RCA) typically involves four main steps – identifying the problem, gathering data, identifying the root cause of the issue, and developing and implementing solutions (Dahlgaard-Park, 2015).
Here is a detailed description of each of these stages:
- Identify the problem/event : To start, it’s crucial to identify the problem or event at hand and involve all relevant stakeholders to clearly understand its scope and impact.
- Gather data : Gathering data is the second step, which includes reviewing documentation, interviewing those involved in the situation, observing processes as well as analyzing available information so that a comprehensive view can be developed.
- Identify the root cause(s) : Thirdly comes identifying root causes. So, various tools such as Five Whys Methodology, Fishbone Diagrams, and Pareto Analysis are used here to analyze collected data before devising solutions addressing each underlying factor identified. This could include process changes/updates training staff or introducing new technologies into play.
- Develop and implement solutions : Last but importantly, we must monitor our chosen strategies’ effectiveness over time by adjusting where necessary if similar issues arise again later down the line.
Pros and Cons of Root Cause Analysis
Root cause analysis (RCA) is an invaluable problem-solving tool that can benefit organizations in numerous ways.
On the pros side, it offers a preventative approach to tackling issues at their source and eliminating them for good.
Plus, its utilization leads to improved processes, better decision-making as well as increased understanding between teams which helps promote collaboration and efficient resource allocation.
Furthermore, addressing root causes also aids customer satisfaction levels by reducing complaints.
Despite all these advantages, though, RCA has some drawbacks.
It takes up time, costs money if specialist tools or outside expertise is required, is quite resource-intensive, has limited scope of effectiveness when dealing with complex problems, and may evoke resistance.
All things considered, however – the benefits provided by root cause analysis significantly outweigh the downsides–particularly in preventing the recurrence of challenges while simultaneously enhancing efficiency.
Root Cause Analysis (RCA) is an invaluable tool for pinpointing the original source of a problem, thus helping to stop it from resurfacing. By getting to its core cause, we can put in place appropriate preventative actions and measures.
It’s widespread across multiple sectors such as healthcare, manufacturing, software engineering, education, construction & retail industries, aerospace/energy, finance, and food service businesses – just to name a few!
To effectively carry out RCA processes, specific approaches could be implemented, like the Five Whys methodology, Fishbone Diagrams, Fault Tree Analyses, Root Cause Mapping, and Pareto Analysis.
All of them provide great insight into why the problem occurred in the first place and allow us to comprehend it thoroughly.
Attar, N. N. (2022). Ideal order management systems for manufacturing industry . London: Sankalp Publication.
Boryczko, K., Szpak, D., Żywiec, J., & Tchórzewska-Cieślak, B. (2022). The use of a fault tree analysis (FTA) in the operator reliability assessment of the critical infrastructure on the example of water supply system. Energies, 15 (12), 4416. https://doi.org/10.3390/en15124416
Charles, R., Hood, B., Derosier, J. M., Gosbee, J. W., Li, Y., Caird, M. S., Biermann, J. S., & Hake, M. E. (2016). How to perform a root cause analysis for workup and future prevention of medical errors: A review. Patient Safety in Surgery, 10 (1). https://doi.org/10.1186/s13037-016-0107-8
Dahlgaard-Park, S. M. (2015). The SAGE encyclopedia of quality and the service economy (Vol. 2). New York: Sage.
Serrat, O. (2017). The five whys technique. Knowledge Solutions, 1 (1), 307–310. https://doi.org/10.1007/978-981-10-0983-9_32
Shinde, D. D., Ahirrao, S., & Prasad, R. (2018). Fishbone diagram: Application to identify the root causes of student–staff problems in technical education. Wireless Personal Communications, 100 (2), 653–664. https://doi.org/10.1007/s11277-018-5344-y
Singh, G., Patel, R. H., & Boster, J. (2021). Root cause analysis and medical error prevention. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK570638/
Vanden, L. N., Lorenzo, D. K., Jackson, L. O., Hanson, W. E., Rooney, J. J., & Walker, D. A. (2014). Root cause analysis handbook. New York: Rothstein Publishing.

- Viktoriya Sus (MA) #molongui-disabled-link Cognitive Dissonance Theory: Examples and Definition
- Viktoriya Sus (MA) #molongui-disabled-link 15 Free Enterprise Examples
- Viktoriya Sus (MA) #molongui-disabled-link 21 Sunk Costs Examples (The Fallacy Explained)
- Viktoriya Sus (MA) #molongui-disabled-link Price Floor: 15 Examples & Definition

- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ 23 Achieved Status Examples
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ 15 Ableism Examples
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ 25 Defense Mechanisms Examples
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ 15 Theory of Planned Behavior Examples
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
MIT Root Cause Analysis
You are here, what is root cause analysis.

A structured approach to indentifying the factors that lead to the outcome of a past event in order to to promote the achievement of better future consequences.
- Root Cause Analysis helps identify what, how and why something happened, thus preventing recurrence.
- Root causes are underlying, are reasonable identifiable, can be controlled by management and allow for the generation of recommendations.
- The process involves data collection, cause charting, root cause identification and recommendation generation and implementation.
Go to Step by Step How To Guide
RCA Toolbox
- Process Map
- Best Practices
- Case Studies
- Video Resources
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Starting the research process
- What Is Root Cause Analysis? | Definition & Examples
What Is Root Cause Analysis? | Definition & Examples
Published on January 6, 2023 by Tegan George . Revised on November 17, 2023.
Root cause analysis is a problem-solving approach that uses the analogy of roots and blooms to model cause-and-effect relationships. Rather than focusing on what’s above the surface, root cause analysis troubleshoots solutions to problems by analyzing what is causing them. Note Similarly to exploratory research , it’s important to remember that root cause analysis does not provide solutions to problems. Rather, it’s one method within a larger problem-solving landscape.
Root cause analysis is a form of quality management, often used in organizational management, quality control, and in healthcare fields like nursing. Root cause analysis can be a helpful study tool for students, too, when used for brainstorming or memorization exercises.
Table of contents
Root cause analysis template, the “5 whys” of root cause analysis, advantages and disadvantages of root cause analysis, other interesting articles, frequently asked questions.
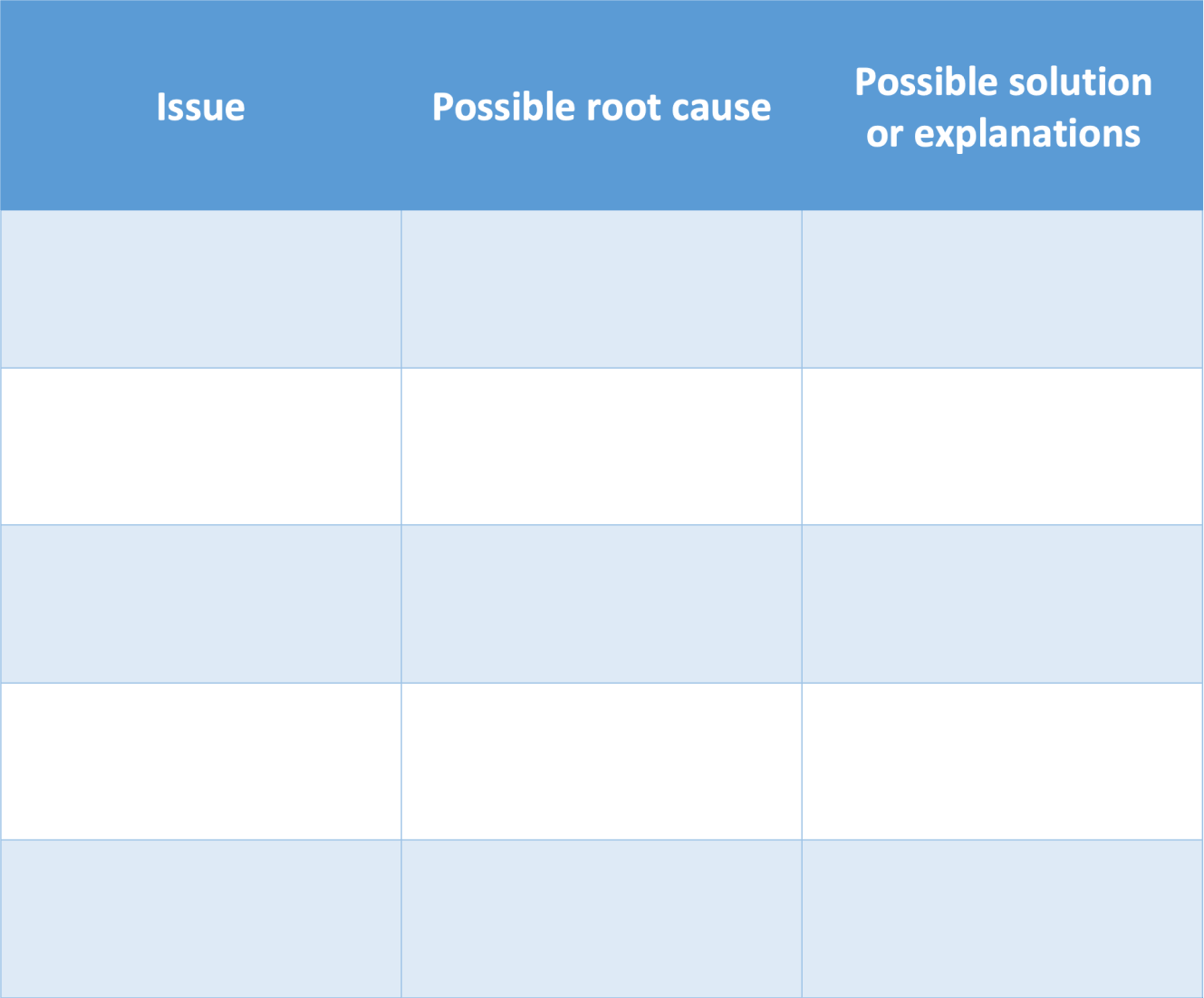
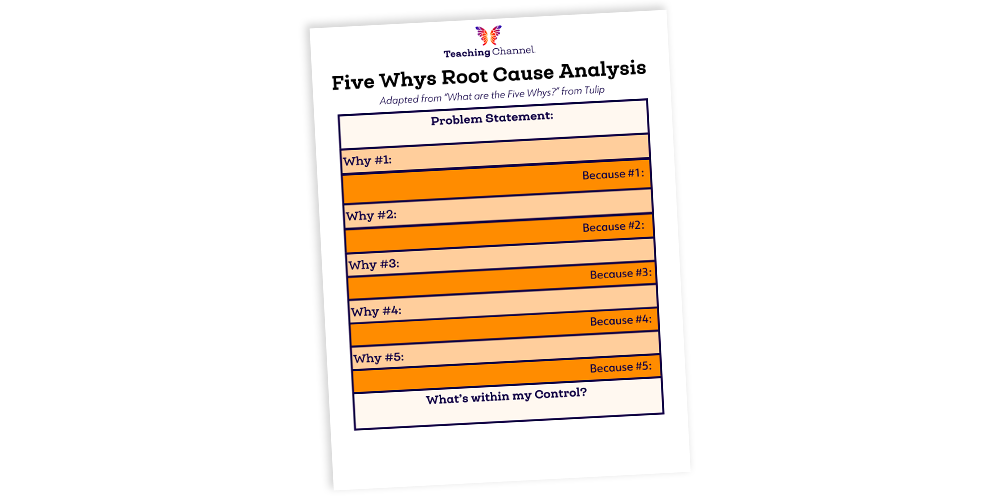
It’s easy to draw root cause analysis charts by hand, on a whiteboard or a big piece of paper. Many people use fishbone diagrams as well, or you can download our template below.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
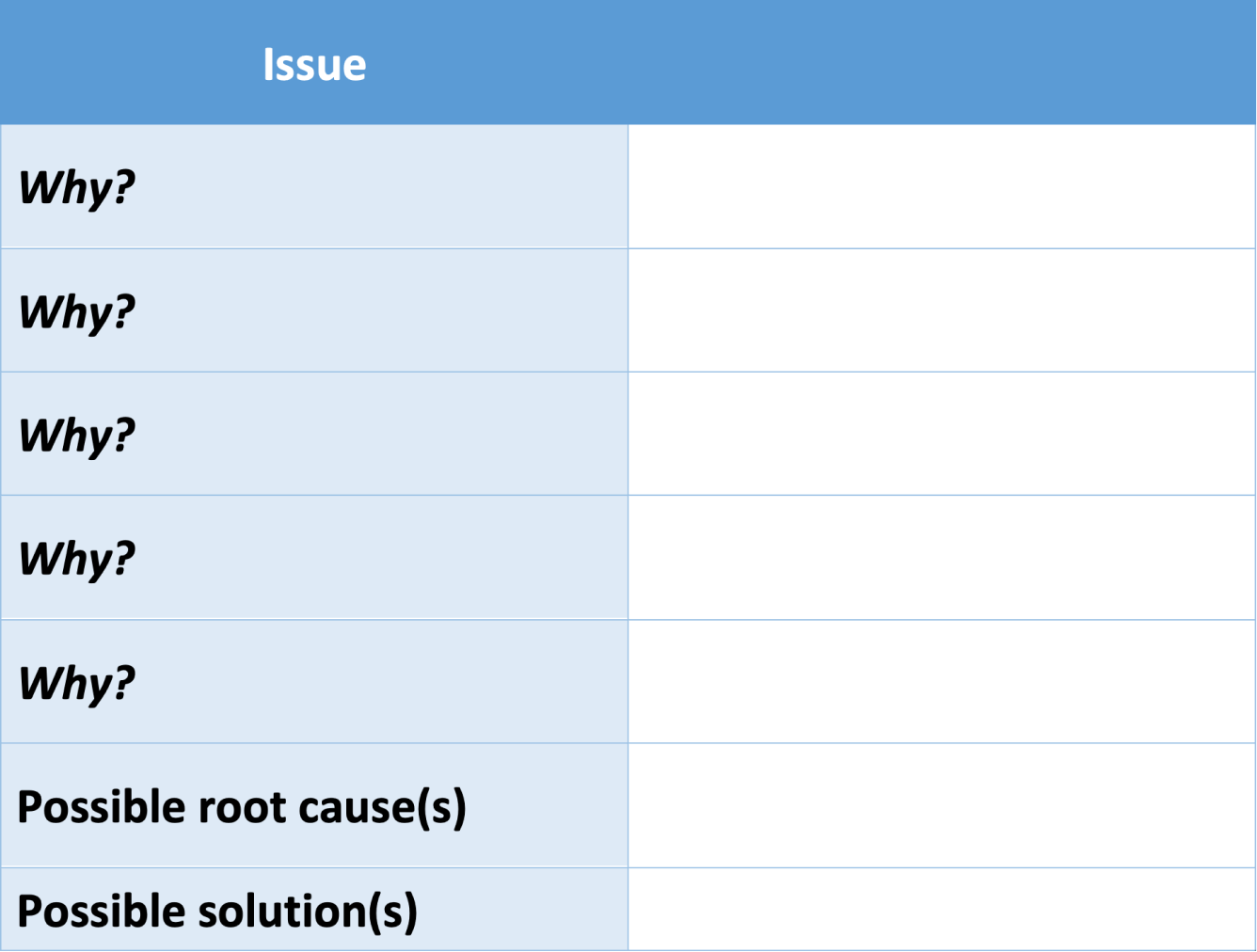
One of the most common ways to conduct root cause analysis is using the “5 Whys” method, popular in lean management. The 5 Whys are an interconnected method of analysis: after defining your problem, you ask “why?” and answer as concisely as possible. The first “why” often leads to the second, which leads to the third, etc.
In short, you continue to ask “why” until the answer provided is no longer a contributor to the broader issue, but a possible solution to that issue. In other words, as you strategize, you’ll sense it’s time to stop when a provided answer has the potential to stop the whole problem from occurring, rather than only one aspect of that problem. This often takes 3-5 “whys” but can definitely stretch out for longer.
You can use this template to map out your whys.
Root cause analysis is a great way to organize your thoughts, but its simplicity leads to a few downsides.
- Great brainstorming tool for individual or group projects.
- Can help identify causal relationships and clarify relationships between variables .
- “5 whys” system can help simplify complex issues and drive possible solutions.
Disadvantages
- Can be overly simplistic, not leaving much room for nuance or variations.
- Path dependence can occur if the wrong question is asked, leading to incorrect conclusions.
- Cannot provide answers, only suggestions, so best used in the exploratory research phase .
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
Methodology
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
Prevent plagiarism. Run a free check.
There are several common tools used for root cause analysis , the most popular of which include fishbone diagrams , scatterplots, and the “5 whys.”
A fishbone diagram is a method that can be used to conduct root cause analysis.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
George, T. (2023, November 17). What Is Root Cause Analysis? | Definition & Examples. Scribbr. Retrieved July 10, 2024, from https://www.scribbr.com/research-process/root-cause-analysis/
Is this article helpful?
Tegan George
Other students also liked, what is a fishbone diagram | templates & examples, how to write a problem statement | guide & examples, how to define a research problem | ideas & examples, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
- Search Menu
- Sign in through your institution
- About BJA Education
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Active and latent errors, executive errors, slips and lapses, planning errors, knowledge based, rule based and mental model mistakes, team-working errors, error within complex systems, incident reporting systems, root cause analysis, 1. getting started, 2. gathering and mapping the information, 3. identifying care and service delivery problems, 4. analysing the information—identifying contributory factors and root causes, 5. generating recommendations and solutions, 6. implementing solutions, 7. writing the report, declaration of interest.
- < Previous
Error and Root Cause Analysis
- Article contents
- Figures & tables
- Supplementary Data
Mhairi Jhugursing, Valerie Dimmock, Haresh Mulchandani, Error and Root Cause Analysis, BJA Education , Volume 17, Issue 10, October 2017, Pages 323–333, https://doi.org/10.1093/bjaed/mkx019
Errors can be defined as an act of commission or omission leading to an undesirable outcome or potentially undesirable outcome.
Error can be classified as active or latent, individual or system based.
Addressing the individual error may prevent the person repeating the same error, whereas addressing latent errors and contributing human factors may prevent an entire organization from making the error again.
In the NHS, incident reporting systems are a form of voluntary staff-led error data collection and collation.
Root cause analysis is a systematic process whereby the factors that contribute to an incident are identified and learned from.
‘Knowledge and error flow from the same mental sources, only success can tell one from the other.’ 1
An error is an act that can lead to an undesirable outcome. Everyone makes mistakes; it is part of the human condition. Cognitive psychologists believe that slips, lapses, and mistakes are inevitable, as they are the price we pay for advanced higher cerebral function. Specifically, a medical error is a preventable adverse effect of care, whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, behaviour, infection, or other ailment. But how do we reconcile this with modern health care, where safe effective patient care is the pinnacle of our practice? James Reason, a British psychologist, founded the framework of error classification and management in health care in the 1990s. As health care has evolved over time, so has our understanding of error and its management. Reason’s work forms the basis of the rapidly expanding field of patient safety. Anaesthesia was one of the first specialities to introduce patient safety guidelines into practice. Patient safety was further highlighted by the Elaine Bromiley case in 2005. This article explores the theory of error occurrence and systems we use to learn from it.
Errors can be defined as an act of commission or omission leading to an undesirable outcome or potential undesirable outcome. 2 Fortunately, not all errors lead to actual patient harm.
The time point the error occurred relative to the error identification, i.e. active and latent errors.
The thought process related to the error, poor planning, or poor execution of a task.
The conscious movement away from established rules within an organization, i.e. violations and malevolent acts.
Team-working errors.
Errors can be thought of as active or latent ( Fig. 1 ).

Active and latent errors diagram.
Active errors occur at the ‘sharp end’ of health care, where an action directly causes an error in real time. 8 , – 10 These errors tend to be person/individual related or immediate equipment failures. Examples include an anaesthetist administering an incorrect drug dose to a patient or not turning on the oxygen flow for pre-oxygenation in a rapid sequence induction of anaesthesia. Active errors are usually picked up quickly at the time of the incident and therefore more easily identified.
Latent errors occur at the ‘blunt end’ of health care. They do not directly cause the error and occur upstream of the event. These errors are wide ranging—the building/room layout, organizational processes, human resources, equipment failure, or medication error. These errors tend to be ‘systems’ related. They are the factors that have contributed to the event. 8–10 For example, many drugs have similar packaging (see Fig. 2 ), and the wrong drug or concentration could easily be administered. Some pumps have multiple steps to their programming, making it difficult to check the correct data have been entered. An example of a human resource error is not enough anaesthetists available to attend a crisis in another theatre during a normal working day.

Drugs with similar packaging.
Latent errors can lie dormant for a long period of time before a situation arises that leads to the error being identified. There has been extensive investment in latent error reduction in many high-risk industries, with human factors engineering playing an important role.
To use an analogy, ‘active failures are like mosquitoes. They can be swatted one by one, but they still keep coming. The best remedies are to create more effective defences and to drain the swamps in which they breed. The swamps, in this case, are the ever present latent conditions.’ 11
An executive error is an active error occurring at an individual level. A task broadly has two stages—the planning phase and the action phase. An executive error occurs when an intended outcome is not achieved because of a deficit in the actions carried out. 8 Executive errors can be further divided into slips and lapses.
Slips are due to attentional failures, usually when undertaking familiar tasks. Familiar tasks have usually been undertaken many times previously and are almost an automatic behaviour, requiring little conscious effort 3 , 8 , 12 . A slip can take the form of intrusions where you are thinking about the management of another difficult case ahead and, for example, inadvertently draw up ephedrine into the intended metaraminol syringe. Slips tend to happen with familiar skill-based tasks.
Lapses are due to memory failures. The tasks involved tend to be complex or have multiple steps, 8 , 12 e.g. forgetting to flush the central venous catheter with 0.9% saline before inserting it or forgetting to give surgical antibiotic prophylaxis prior to making an incision (see Fig. 3 ).

Summary of error types. Adapted from St Pierre et al. 8
A planning error is a form of active error, where the intended outcome is not achieved because of a deficit in the planning before execution of the task and is termed as a mistake. Planning relies on thought processes, and it applies largely to unfamiliar tasks. It is a conscious effort and requires more focus and energy than automatic familiar tasks. Problem solving is required to formulate a plan, and there are three common cognitive tools used to facilitate the process: knowledge based, rule application, and a mental model. 8 , 12
Knowledge-based mistakes are generated by lack of facts related to the problem. 8 , 9 , 12 For example, suxamethomium can trigger malignant hyperthermia; and patients with diabetes can have gastric autonomic neuropathy, increasing the risk of acid reflux and aspiration.
Rule application concerns the use of a set of learned guidelines. Mistakes can occur in the misapplication of a ‘good’ rule, e.g. giving a beta-blocker to a patient with fast atrial fibrillation to control the heart rate, but the patient has asthma. Using the ‘wrong’ rule also causes mistakes, 8 e.g. using the pneumonia guidelines to treat a patient with pulmonary embolus.
Mental models are psychological representations of a situation. We often rely on previous experience when encountering a new situation and tend to use a mental model that best fits when we previously felt in control. However, this may not be the reality of the situation. 8 For example, a general anaesthetic is administered to an obstetric patient because of inadequate epidural anaesthesia for urgent Caesarean section. The patient becomes hypotensive and is resuscitated with i.v. fluids. Previous experience has been of obstetric hypotension caused by maternal haemorrhage, and aggressive blood transfusion is commenced. The obstetricians have achieved haemostasis, but the mental model persists and further fluids and blood products are given for presumed occult blood loss. The blood pressure remains low and the oxygen saturations drop as fluid overload manifests. The mental model has falsely reassured the anaesthetist who has overlooked or dismissed other causes of hypotension, such as a ‘high’ regional block. Mental models should not be relied upon and should be frequently re-evaluated.
As an anaesthetist progresses through his/her career, the likelihood of particular error types changes. In the early stages of a doctor’s career, knowledge-based errors are more likely. As the novice advances and acquires his/her basic competencies his/her practice is guided by a basic set of rules, hence rule-based error usually occurs at this point. As an anaesthetic consultant, the majority of activities have become automatic skills, and slips and lapses can creep in. 8
Slips, lapses, and mistakes are unintentional behaviours that may lead to patient harm. Violations differ as they are deliberate acts that deviate from the accepted guidelines of safe practice. In some rare instances, they are malevolent acts, where staff deliberately cause harm to patients, equipment, or other staff members. However, the majority of violations are committed with the intention of making a task easier or quicker, despite falling outside the safety guidelines. Such ‘shortcuts’ may on the surface seem to be a better trade-off between efficiency and risk but may cause patient harm. Continued violation of a safety protocol at an individual or department level will lead to a bare minimum safety margin, where serious harm could occur. 8 An example would be preoperative assessment of elective cases in the anaesthetic room. This would be time saving but would need to be balanced against the risk of pressure to proceed with surgery, even with insufficient investigations. In most occasions, all required information will be available and anaesthesia will proceed safely.
Active errors from the individual can be minimized by the use of checklists, briefings, guidelines, structured handovers, read backs, and double checks, ‘Do not enter—anaesthesia in progress’ signs, and simulation training (see Table 1 ).
Latent errors within a system can be minimized by automated systems, standardization of equipment and drugs, and optimal equipment design with forced functions (i.e. equipment or systems that only allow specific standardized options to minimize error) (see Table 2 ).
Measures to reduce active errors 6 , 9 , 10 , 15
| Checklists | World Health Organization (WHO) surgical checklist, Safe Anaesthesia Liaison Group (SALG) ‘Stop Before You Block’, anaesthetic machine check, rapid sequence induction checklist, transfer checklist. |
| Briefing and debriefing | Theatre team planning and review of surgical list. |
| Guidelines | Association of Anaesthetists of Great Britain and Ireland (AAGBI) – anaphylaxis, malignant hyperthermia, local anaesthesia (LA) toxicity, Difficult Airway Society (DAS)— difficult intubation. |
| Handovers | Obstetric ‘Sick patients, At risk, Follow-ups, Epidurals’ (SAFER) handover, postoperative paediatric intensive care unit handover. |
| Read backs | Patient details—name, date of birth, hospital number, blood results. |
| Simulation training | Crisis resource management—also termed team resource management, human factors training, anaesthetic critical incident management, emergency airway management |
| Double checks | Drug calculations, drug infusion preparation, controlled drug administration. |
| Checklists | World Health Organization (WHO) surgical checklist, Safe Anaesthesia Liaison Group (SALG) ‘Stop Before You Block’, anaesthetic machine check, rapid sequence induction checklist, transfer checklist. |
| Briefing and debriefing | Theatre team planning and review of surgical list. |
| Guidelines | Association of Anaesthetists of Great Britain and Ireland (AAGBI) – anaphylaxis, malignant hyperthermia, local anaesthesia (LA) toxicity, Difficult Airway Society (DAS)— difficult intubation. |
| Handovers | Obstetric ‘Sick patients, At risk, Follow-ups, Epidurals’ (SAFER) handover, postoperative paediatric intensive care unit handover. |
| Read backs | Patient details—name, date of birth, hospital number, blood results. |
| Simulation training | Crisis resource management—also termed team resource management, human factors training, anaesthetic critical incident management, emergency airway management |
| Double checks | Drug calculations, drug infusion preparation, controlled drug administration. |
Measures to reduce latent errors 9 , 10 , 15
| Automated systems | Real-time electronic anaesthetic charts, bar code blood product checks, anaesthetic machine checks. |
| Standardization | Patient controlled analgesia (PCA) and potassium drug infusions prepared by pharmacy with standardized concentrations, syringe tips—specific to epidural/spinal anaesthesia, catheter mounts 15/22 mm connectors. Schrader probes/non-interchangeable screw thread connections. |
| Equipment design and function | Monitors with visual data and audio data (including pulse oximetry saturation percentage and tone). Monitor display arranged so that it is easy to see basic vital measurements. Target-controlled infusion (TCI) pumps that are easy to programme and review data before proceeding. Giving pre-programmed options of TCI protocols, e.g. Marsh and Minto models. PCA pumps with preset standardized programmes. |
| Automated systems | Real-time electronic anaesthetic charts, bar code blood product checks, anaesthetic machine checks. |
| Standardization | Patient controlled analgesia (PCA) and potassium drug infusions prepared by pharmacy with standardized concentrations, syringe tips—specific to epidural/spinal anaesthesia, catheter mounts 15/22 mm connectors. Schrader probes/non-interchangeable screw thread connections. |
| Equipment design and function | Monitors with visual data and audio data (including pulse oximetry saturation percentage and tone). Monitor display arranged so that it is easy to see basic vital measurements. Target-controlled infusion (TCI) pumps that are easy to programme and review data before proceeding. Giving pre-programmed options of TCI protocols, e.g. Marsh and Minto models. PCA pumps with preset standardized programmes. |
No department is error proof. Reason proposed the ‘Swiss Cheese’ model to describe the trajectory of an error (see Fig. 4 ). 9 Multiple safeguards are put in place to avoid errors in a system. Each layer of protection will have an area of weakness, representing a hole in the defence. With multiple layers, even if an error breaches one layer, the next layer will catch the error before it causes patient harm. This model can be 100% effective in a static environment, but the NHS is a complex dynamic system with multiple ‘moving’ layers of protection, thus at some point the ‘holes’ in each layer can align, allowing a straight path to patient harm. There are, however, limitations to the ‘Swiss Cheese’ model in that it implies linear determinism. While that may be true in some industries such as nuclear and aviation, in health care it seldom is, as events rarely unfold in a single straightforward pattern, and are usually much more complicated and interrelated. 3 , 8 , 12 A comparably complex situation to health care is in the prediction of extreme weather events. It is not always possible to predict the occurrence of a severe hurricane or flood, as there are numerous factors that interplay to lead to one, but once one has occurred, the factors leading up to it can be analysed in retrospect in great detail.

Swiss Cheese model. 9
Error theory is constantly evolving. Suggested theories and solutions are more applicable to a static environment; however, health care is a dynamic environment. An expanding population, with increasing levels of co-morbidity, coupled with demand outstripping resources, means the health care environment will only get more complex over time. Kinnear proposed a different approach accepting the fluidity of the health care environment and focusing on our innate ability to problem solve through resilience engineering. 16 This is examining what works well in this challenging environment, in addition to went wrong. Resilience engineering involves building a flexible organization that anticipates the dynamic nature of errors and continually revises risk models to reduce errors before they occur. 11
Errors will occur within every health care system. It is important that these errors are identified and lessons drawn from these cases to improve patient safety. Incident reporting systems (IRS) collect error data with the aim of facilitating learning and improving patient safety. They are passive processes where data are voluntarily reported by staff on the front line. Voluntary incident reporting is highly variable and does not truly reflect the incidence of errors, which are generally under-reported within health care. However, these passive systems are relatively inexpensive and empower staff to identify and learn from error. If lessons are appropriately disseminated to the right people, the required changes can be made to prevent recurrence. Increased reporting can be encouraged with an open ‘fair blame’ culture ensuring timely feedback and improvements. 7 , 14 A ‘fair blame’ culture achieves a balance of openly investigating the factors leading up to an incident and our individual responsibility and behaviour as health care professionals to maintain good practice and safety. In the UK, 75% of Trusts use the Datix web-based software programme for incident reporting. Once reported, the process of learning and improving patient safety begins with root cause analysis (RCA). There are two general approaches to error investigation: person based and system based.
The person-based approach focuses directly on the unsafe act committed by the person causing the incident and implies that the error is specific to that individual, separating the incident from the latent errors and human factors contributing to it. Unfortunately, the person-based approach is prevalent throughout many organizations. 8 With this approach, it is easier to blame an individual for his/her carelessness, inattention, recklessness, or lack of education. This tends to lead to a ‘naming, blaming and shaming’ culture, where if a similar circumstance were to occur again, the likelihood is that the same error would happen. In addition, the morale and confidence of the individuals involved may be permanently damaged. This is not an effective approach to error reduction in health care. The Berwick Report (2013) on patient safety in the NHS stated we should ‘abandon blame as a tool’. 17
The basic premise in the system-based approach is that humans are fallible and errors are expected, even in the best organizations.
The systems-based approach is far more applicable to the NHS and considers the organizational processes and chain of events that lead to the error. Errors are seen as consequences rather than causes, having their origins not so much in the perversity of human nature as in the ‘upstream’ systemic factors. 11 Countermeasures are based on the assumption that though we cannot change the human condition, we can change the conditions under which humans work. RCA examines both aspects, but with particular emphasis on the systems-based approach. 8
RCA is the structured, thorough investigation of a patient safety incident to determine the underlying causes and contributing factors, and then analyse these to draw out any learning points. 7 The learning points can be actioned to reduce the chance of the same or similar incident reoccurring. The Berwick Report stated as its main objective regarding patient safety, ‘A promise to learn—a commitment to act: improving the safety of patients in England’. 17 The most widely adopted RCA template is from the National Patient Safety Agency (NPSA), which is detailed below. The process of RCA can be broken down into seven steps 18 (see Fig. 5 ).

The RCA investigation process.
The RCA investigation process
Worked Example
Incident Report System (Datix) summary from theatres:
Vascular surgery emergency open abdominal aortic aneurysm (AAA) repair (failed endovascular aortic repair (EVAR)): Incorrect dose of heparin administered during surgery, patient suffered coagulopathy causing major surgical haemorrhage and cardiovascular instability requiring multiple blood product administrations. Patient admitted to intensive care unit postoperatively. Patient remains intubated with high oxygen requirements secondary to transfusion related acute lung injury (TRALI) and is receiving renal replacement therapy due to acute renal impairment. Anaesthetist who administered heparin had drawn up the incorrect dose. There are two different heparin vial concentrations in the anaesthetic room drug cupboard, heparin 100 units/ml and 1000 units/ml.
Level 1 – No harm (‘near miss’)/low harm/moderate harm. A concise investigation usually handled by one local person, comprising a one-page summary.
Level 2 – Severe harm or death. A comprehensive investigation, an in-depth assessment requiring a multidisciplinary team, which was not involved in the incident, or in the locality or directorate. There may be expert opinion sought.
Level 3 – Severe harm, death, or public interest. As above, plus incidents of public interest or notifiable serious incidents (e.g. never events). These investigations are carried out by investigators external to the organization.
The RCA team will routinely comprise a person trained in RCA, expert(s) in the incident field, an administrator, and a non-executive person (layperson or patient representative). 18
Patient safety incident Level 2 (severe harm), requiring comprehensive investigation by RCA team. RCA team assembled. Consultant anaesthetist (not involved in the incident), consultant vascular surgeon (not involved in the incident), medical secretary, pharmacist, and patient advisory liaison officer.
This step is about gathering all relevant facts surrounding the incident, avoiding opinions and other bias, e.g. the cultural bias ‘this is the way it has always been done here’. The sources of information may include medical notes, staff statements, staff rotas (to ascertain staff numbers and skill mix), interviews, local and national policies, guidelines and inspection of equipment and drugs. Interviews can be challenging, highly emotive situations and individuals frequently have poor or altered event recollection. Group interviews suffer from hierarchical impedance whereby in a group of nurses and doctors, nurses may tend to speak up less frequently. Similarly, in a mixed group of junior doctors and consultants, the junior doctors may be less likely to express their concerns. It is important to have an experienced facilitator during group interviews with sensitive and concise questioning to obtain the facts.
All facts should be collected, including conflicting information. Expert opinion should be obtained. Data gaps should be identified and areas of good practice should be identified. This is a fact-finding mission at this stage of the RCA, and the temptation to analyse the data should be resisted. 17 The mapping of information can be recorded via a tabular timeline or a time/person grid (see Worked example on the previous page). 18
Care delivery problems (CDPs) and service delivery problems (SDPs) include all acts of commission and omission. CDPs generally involve failure to monitor, observe, or act. 18
Not noticing the intravenous cannula has ‘tissued’ during total intravenous anaesthesia (TIVA).
A trainee not escalating an ASA 4 cardiovascularly unstable vascular patient to the consultant before commencing anaesthesia.
Not giving antibiotic prophylaxis to a patient undergoing hemiarthroplasty, with subsequent joint infection.
Failure to ask for assistance when spinal anaesthesia has failed in a category 1 Caesarean section with a delay in delivery, resulting in a neonate with poor Apgar scores.
The decision to skip the team briefing in the morning before the list starts, which subsequently leads to a specific piece of surgical equipment not being available for a difficult case.
Unintentionally using 2% instead of 1% propofol in the TIVA pump, causing cardiovascular instability in a patient.
The administration of neat potassium chloride solution in a paediatric burette to an adult patient causing an unpredictable infusion rate, resulting in cardiac arrhythmias.
Continued shortage of central venous catheters in the operating theatre area.
Inadvertently giving local anaesthetics drugs intravenously, causing cardiovascular instability.
Inadequate handover of septic patient, causing delay in treatment.
CDP: Failure to identify correct vial of heparin for vascular procedure by anaesthetic registrar, anaesthetic registrar failure to register, or read the heparin vial label correctly. Consultant failed to check the heparin concentration before administration.
SDP: Two different concentrations of heparin available beside each other in the anaesthetic drug cupboard. Anaesthetic registrar had drawn up multiple drugs over short space of time, while on phone to haematology department.
Contributory factors:
Equipment and resources: Two different concentrations of heparin vials available in the anaesthetic drug cupboard with similar packaging and labels.
Patient factors: Emergency ASA 4e patient cardiovascularly unstable requiring multiple anaesthetic interventions.
Individual factors. Anaesthetic registrar fatigue.
Task factors: Anaesthetist carrying out multiple tasks at once.
Communication factors
Consultant did not ask to see the vial of heparin to check the dose he was administering. Poor communication between surgeon and anaesthetist leading to delay in identification of the problem—assumption excessive haemorrhage was due to surgical trauma, assumption anaesthetist aware of unusually excessive bleeding. Delay in direct communication with haematologist on-call to receive advice about coagulopathy management. No allocated person to liaise with haematology team.
Team and social factors
Multiple activities occurring—additional anaesthetic staff available, but not requested. Theatre staff unaware of error until late in chain of events. If had information earlier could allocate more staff to assist.
Education and training factors
Anaesthetic registrar not aware of two different concentrations of heparin available as he/she is new to the hospital.
Working c onditions
Error occurred during busy night shift, but appropriate level of staffing available.
Organizational and strategic factors
Drugs available in anaesthetic cupboard vary between each theatre and different packaging for same drug.
Root cause:
Equipment latent error
Heparin drug vials of different concentrations found together with similar packaging and similar labels.
Active i ndividual slip
Not reading fully the label on the heparin vial before drawing the drug up by the anaesthetic registrar.
Routine violation
Consultant anaesthetist not rechecking the drug vial before administering to patient (as he did not personally draw up the drug).
Reliance in part on mental models by surgeons and anaesthetists leading to delayed recognition of the error.
Team work error
Poor communication between all groups involved, deficient situational awareness, suboptimal task prioritization, and task allocation

Using the Fishbone (Ishikawa) Diagram to analyse the information- identifying the contributory factors and root causes.
Human actions, e.g. teamwork, handovers, and skills.
Administrative actions, e.g. procedures, policies, guidelines, training, and supervision
Physical actions, e.g. similar product packaging changed and equipment with forced functions. 18
Solutions with a large impact within an entire organization are often more difficult to achieve than more localized ones. Therefore, solutions that work on both levels should be considered to achieve optimal safe working environments and practices (see Fig. 7 ). 18 Constructing a Pareto chart may be useful to focus interventions to gain maximum benefits. A Pareto chart is a combined bar and line graph, which indicates the reduction in an event occurrence relative to specific interventions.

Generating recommendations and solutions.
Physical action: Have single-set concentration of heparin for intraoperative boluses available in the anaesthetic drug cupboard in theatres, with the second concentration for infusions in recovery drug cupboard within the next 2 weeks. This should be standardized across the trust within next 4 months.
Review and reduce drug packaging similarities across trust in all clinical areas over next 12 months.
Human actions: leadership and team working training for theatre staff, focusing on human factors in crisis situations. Training to be initiated within the next 3 months.
Administrative actions: Major haemorrhage protocol review, focusing on improving line of communication between theatres, maternity, emergency department, and haematology team. Aim to complete review within next 4 months.
Implementing a solution is an ongoing dynamic process involving communication, dissemination, diffusion, adoption, spread, and sustainability. An action plan must be specific, measurable, achievable, relevant and timely (SMART). A common template used is an Action Plan Document (see Worked example on the next page). This document encourages the consideration of common factors required for a successful solution implementation. 18 A successful solution implementation is evidenced by measurement of the intended effect. This is akin to a quality improvement project where the Plan, Do, Study, Act (PDSA) cycle continuously assesses and refines the value of the activity.
There are report templates (concise, comprehensive, and external) on the NPSA website; however, each trust will have its own modified template. It is important when analysing investigation findings to be aware of, and try to avoid, hindsight bias and outcome bias. Hindsight bias is the tendency for people with the ‘benefit of hindsight’ to falsely believe, once all the facts become clear, that the actions that should have been taken to prevent an incident seem obvious, or that they could have predicted the outcome of the event. 18 Outcome bias is the tendency to judge a past decision or action by its success or failure, instead of based on the quality of the decision made at the time. No decision maker knows for sure whether or not the future will turn out for the best following any decision they make. Individuals whose judgements are influenced by outcome bias can hold decision makers responsible for events beyond their control. 18 Similarly, if an incident leads to death it is often considered very differently and critically, compared with an incident that results in no harm, even where the incident or error is exactly the same. When people are judged one way when the outcome is good, and another when the outcome is poor, accountability levels become inconsistent and unfair. To avoid the influence of outcome bias, one should evaluate the decision or action taken at the time it was taken, and given what was known or going on at that time, irrespective of the successful or failed outcome. When producing the report, it is important to bear in mind which differing groups will have access to and be reading the report. This may include clinical staff, patient(s) involved and their relatives, hospital patient safety committee, hospital board, Department of Health, coroners, solicitors, general public, and media. It is therefore important to set the right tone, format, and style for all the interested parties. The report must be clear, concise, logical, and show an open and fair approach, and be in the third person. The report should be anonymized and avoid negative or inflammatory descriptors. It is best to record facts and reasoned conclusions, not opinions and assumptions. Link care and service delivery problems with their root cause and then demonstrate the shared learning derived from that. 18 The RCA report must be completed within 60 days of identification of the incident by the patient safety team.
The amalgamation of the entire RCA, ensuring tone, language, and data, are suitable for each group of people who may be reading it. The report should include the analysis, all recommendations and actions with time frames, and identified personnel who will be responsible for ensuring compliance.
To err is human, to cover up is unforgivable, to fail to learn is inexcusable. 19
None declared.
The associated MCQs (to support CME/CPD activity) can be accessed at http://www.oxforde-learning.com/journals/ by subscribers to BJA Education .
Mach E. Knowledge and Error . Dordrecht, Holland: Reidel, 1976 (originally published in German , 1905 )
Google Scholar
Google Preview
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 33 – 51
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 21 – 31
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 149 – 59
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 111 – 23
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 303 – 19
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 233 – 53
St Pierre M , Hofinger G , Buerschaper C , Simon R. Crisis Management in Acute Care Setting , 2nd Edn. New York: Springer , 2015 ; 41 – 59
Gregory B , Kaprielian VS. Anatomy of Error Module Duke University of Medicine. Available from http://patientsafetyed.duhs.duke.edu/module_e/module_overview.html (accessed 3 June 2016)
Wheeler SJ , Wheeler DW. Medication errors in anaesthesia and critical care . Anaesthesia 2000 ; 60 : 257 – 73
Reason J. Human error: models and management . BMJ 2000 ; 320 : 768 – 70
Zhang J , Patel VL , Johnson TR , Shortliffe EH. A cognitive taxonomy of medical errors . J Biomed Inform 2004 ; 37 : 193 – 204
Fortune PM , Davis M , Hanson J , Philips B ; Advanced Life Support Group . Human Factors in the Health Care Setting . New Jersey, USA, London, Oxford: Wiley-Blackwell , 2013 ; 20 – 35
Carthey J , Clarke J. Implementing human factors in healthcare PDF. Patient Safety First Group. Available from www.weahsn.net/wp-content/uploads/Human-Factors-How-to-Guide-v1.2.pdf (accessed 3 June 2016)
Human Factors and Managing Error . NHS Education for Scotland. Available from https://learn.nes.nhs.scot/Resource/View/800 (accessed 3 May 2017)
Kinnear J. Presentation—Damage Limitation—Minimising Unintentional Harm: Complexity, Team Working & Human Factors . The Royal College of Anaesthetists, Patient Safety in Peri-Operative Practice , 2014
Berwick D. A Promise to Learn—A Commitment to Act. Improving the Safety of Patients in England. Commissioned by NHS England, 2013
Root Cause Analysis . National Patient safety Agency. Available from www.nrls.npsa.nhs.uk (accessed 3 June 2016)
Donaldson L. Twitter account quote. 2011
Email alerts
Affiliations.

- Online ISSN 2058-5357
- Print ISSN 2058-5349
- Copyright © 2024 The British Journal of Anaesthesia Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Lavinia Group
- Insight Education Group
- Course & Account Access
- Video Platform Account Access
- Graduate-Level Courses
- Fast Track Courses
- Course Bundles
- Certificates
- Flex Credit Courses
- Hours-Only PD Courses
- Advanced Degrees
- Course Topics
- Course Formats
- Term Calendar
- University Partners & Transcripts
- Course Pricing
- Pay as You Learn
- Group Registrations
- Group Savings
- Bundle Savings
- New Customer Discounts
- Refer & Earn
- Connecticut
- District of Columbia
- Massachusetts
- Mississippi
- New Hampshire
- New York City
- North Carolina
- North Dakota
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- West Virginia
- How it Works
- Become a Group Leader
- Start a Group
- Teacher Exemplar Video Library
- Video Coaching & Learning Platform
- School & District PD
- New Teacher Course
- Substitute Teacher Course
- Build Your Program
- Video for Educators in Training & Higher Ed Faculty
- Case Studies
- Book a Demo
- Chat With Us
- In the Press
- Downloadables
- Lesson Plans
- Presentations
- Video Blogs

July 8, 2024
Julie Kuntz
“Five Whys” Analysis: Finding the Roots of Teacher Sustainability
Summertime is the time to recharge. Time to read a book (for pleasure!), plant in your garden, and sleep in. The summer feels good . Every summer, I think fondly about teaching. All those frustrations (the missing assignments, broken wifi connections, student behaviors, subbing on my prep) disappear as summer rolls around, and by the fall, I always arrive hopeful, happy, and refreshed.
But if you ask me how I feel about teaching in December? That’s an entirely different story.
Fall teaching workshops are often filled with reminders to “find your why.” Personal reflections asking you, “Why do you teach?” or “Why do you believe in education?”
Unfortunately, there is another why question that remains unanswered: if I am passionate about education, then why does this work feel unsustainable?
Perhaps we don’t need help finding our why as much as we need help figuring out the how :
- how can I make education a sustainable profession for me?
- how can I operate in a system that often feels inequitable and contradictory to my values?
- how can I find happiness and peace when the day-to-day operations of school often feel quite the opposite?
To answer these questions we need to find the roots of the issues. A Root Cause Analysis can help us do this by inviting us to ask “why” as an entry point for digging deeper rather than a destination for accepting the challenges of education because we care about our students. The Five Whys is a powerful tool to help us do this.
For example, my problem could be stated as: Teaching does not feel sustainable for me. I need to start following a trail of whys to investigate further. It might look something like this:
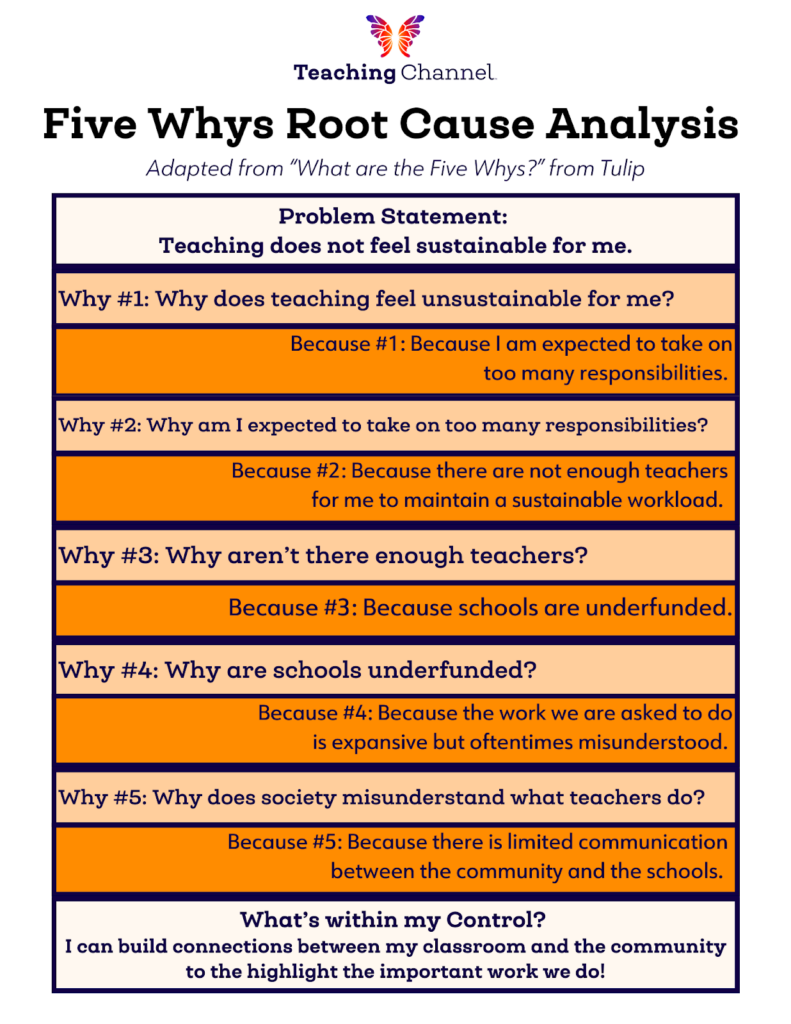
After digging Five Whys deep, I am now beginning to uncover some root causes and identify which whys I have agency to change. For example, I might not have control over the lack of school funding, but I have control over communication between the community and my classroom. Use this template to view the above example and then create a Five Whys analysis to answer your own questions about education.
This does not mean all roots grow the same! Sometimes a Five Whys analysis will show there is nothing in your control to change. Or you might hit a dead end after three whys, or barely scratch the surface after six: that’s okay! Remember, the purpose of the Five Whys is to discover that sustainability challenges are more complex than repeating a teacher mantra every morning on our drive to work or getting “I love my students” tattooed on our arms.
Digging deeper into the whys will help us eventually arrive at the hows of our work. By discovering our hows, we can uncover ways to do our work in sustainable ways, to not only believe in our why, but to live it.
About the Author

Julie Kuntz holds a B.A. in English and a Master’s in Education. Drawing on her years as a Middle School ELA Teacher, Julie develops content that is practical and highly engaging! Additionally, she is passionate about fostering equity in schools.
Fun Fact: Julie and her husband own a custom home renovation company, Custom by Kuntz!
Related Topics in Educator Wellness
Related content.

Marcee Harris
Powerful Vocabulary Activities to Boost Reading Comprehension

Sarah Murphy
3 Activities for Practicing AI Literacy
Search the k12 hub, more from teaching channel.

3 Mistakes I Made in My First Year of Teaching
It was a cloudless day in early September as I stood at my classroom door greeting students with a muddled mix of excitement and terror

Go “Beyond the Book” in a Brand New Series
Have you ever read a Young Adult (YA) text, and known from the minute you finished it that it would be the perfect book to

The Surprising Power of Play to Get Kids Moving and Brains Booming
Have you ever noticed how kids seem to learn best when they’re moving? There’s a reason for it! Research shows that movement and play are
Recommended Courses
Reclaiming your passion for teaching with balance and bandwidth, educator wellness, goodbye teacher burnout, welcome teacher wellness.
Flex Credit
Connection and Calming Strategies for Today’s Teachers

Want to partner with us?
We’re always looking for new authors! If you’re interested in writing an article, please get in touch with us.
Subscribe to our Newsletter!
Get notified of new content added to K12 Hub.
- I am a Teacher or Teacher leader
- I am a District or School Administrator or Leader
The Importance Of Root Cause Analysis
Do you often find that you are faced with a problem that seems unsolvable? In that case, you’re not alone….

Do you often find that you are faced with a problem that seems unsolvable? In that case, you’re not alone.
When we don’t get the desired outputs or results from a business plan, we’re quick to point fingers. Sometimes, we blame the plan and adopt a new strategy. However, problems persist.
This is why it’s important to find the root cause of problem areas before jumping to half-baked conclusions. Let’s start by understanding the meaning of root cause analysis and learn different ways to avoid repetitive mistakes.
Meaning Of Root Cause Analysis
To define root cause analysis, we must first understand the term ‘root cause’. A root cause is a basic or fundamental cause of something. It often needs to be permanently eliminated through improvement. Simply put, RCA is the core issue that sets the entire cause-and-effect in motion, thereby leading to problems further down the line.
RCA or Root Cause Analysis is an analytical tool, technique, or process used to get to the root cause of the problem. It’s a fundamental tool in the journey of continuous improvement. In itself, root analysis may not produce any solutions but by making it a part of larger problem-solving efforts, quality improvement can be achieved.
Why Perform Root Cause Analysis?
Root analysis helps us look beyond the superficial cause-and-effect and takes us to the bottom of the failed systems or processes that caused issues in the first place. Unless we determine the real root of any problem, the problem is likely to repeat itself. The process of root cause analysis comes with certain end goals and benefits:
The first goal of root analysis is to discover the core issue or the root of a problem or event
The second goal is to understand how to fix the underlying issues and learn from mistakes
The third goal is to apply our learnings so that the patterns can be systematically used to prevent future issues
Root analysis teaches us that identifying the core process or the system isn’t enough. Unless you actively deploy the learnings from the analysis, the situation may not improve. For example, if you hurt your knee during a soccer match, root cause analysis might suggest that the ligaments around your knee are weak. So, you may be advised to start wearing a knee-pad to minimize the risk of future injuries.
Principles Of Root Cause Analysis
There are a few core principles that can improve the quality of analysis and help to gain trust from your peers, coworkers, or clients. The principles that guide effective root cause analysis are:
Instead of focusing on the indicators, try and correct the root cause
Always address the surface-level signs/indicators for short-term remedies
It’s important to remember that there can be multiple root causes for the same situation
Instead of being critical about ‘who’ was responsible, try understanding ‘how’ and ‘why’ something happened
Never jump to hasty conclusions. Take your time and be methodical about finding sound cause-effect evidence to back up your root cause claims
Support your corrective course of action with ample information
Consider how to prevent or adopt the root cause to your advantage in the future
Tools Of Root Cause Analysis
Now that we’ve established how to apply the basics of root cause analysis, let’s find out how we can use them effectively. Organizations are encouraged by people with good problem-solving and decision-making capabilities to bring sound solutions to the table.
Here are a few strategies and techniques to conduct effective RCA:
1. The Five Whys
One of the most common and effective ways of performing root cause analysis is the Five Whys analysis. You evaluate a problem by asking the question ‘why’ five times. It’ll help you identify which layer of the problem or situation needs to be revised, corrected, rebuilt, or rethought. The five whys serve as a way to steer away from assumptions. Choices or solutions become clearer after each ‘why’ question is asked. The answer to the last ‘why’ should ideally lead you to the root cause you need to address.
2. Change/Event Analysis
Another handy technique of using the root analysis method is to study or analyze the changes that led to an event. This method is especially fruitful when there’s a large number of causes. Instead of looking at a specific instance, we step back and try to analyze situations over some time.
The process of change/event analysis includes four essential stages:
List every potential cause that led to an event. Take into account the times when a change has occurred, for better or worse. For example, the last “Grand Sale” day at your company was a huge success. You may want to note down all the touchpoints with every major customer.
Categorize each change or event by the amount of influence you had over it. It can be known or unknown, internal or external. For example, offering a heavy discount is an internal factor and the last day of the quarter can be an external factor.
A significant chunk of the analysis happens in this stage. Every event is analyzed to figure out whether there was a correlating, unrelated or contributing factor. For example, a new idea can be a contributing factor but the end of the quarter is an example of an unrelated factor because it can’t be controlled.
In this last stage, we can choose to replicate or remedy the root cause. For example, if new ideas and initiatives are boosting sales, then organizing brainstorming sessions may help. You can decide to replicate the root cause of success.
3. Fishbone Diagrams
The fishbone diagram, also known as the Ishikawa diagram, is a popular root cause analysis technique. It’s named so because it resembles a fish’s skeleton. Using it, you can draw a mental map that’ll help you identify the underlying factors. The diagrams typically start with the spine, i.e., the problem. Each bone branches out to include smaller bones, indicating several categories of causes and sub-causes. As each branch is analyzed, we dig deeper into possible causes. This is how we get closer to the main sources of the issue or problem at hand. For example, if your category is ‘people’, you may want to look at ‘leadership’, ‘training’, ‘staffing’.
4. Pareto Analysis
The Pareto analysis is a well-defined root cause analysis tool. It takes a statistical approach to decision-making. It’s based on the principle that 80% of effects come from 20% of causes. This 80/20 rule simply means that 20% of the work creates 80% of the results. There is a risk of focussing too much on trivial problems in the process of reviewing or analyzing. We must focus our energies on the ‘vital few’ as opposed to the ‘trivial many’. ( https://rentalsfloridakeys.com/ ) For example, you may find that 20% of your female customers are the cause of 80% of your sales. However, it doesn’t mean that you focus all your marketing efforts only on your female customers.
5. Kepner Tregoe Method
Also known as the KT Method, the Kepner Tregoe Method is a powerful problem-solving tool. Developed by two pioneers of rational decision-making, Charles Kepner and Benjamin Tregoe, this working method has been proven to produce results. Organizations often face the pressure of solving problems. There are many opinions on what the right approach to solving them should be. The KT method is a crucial analysis tool where the ‘problem’ is disconnected from the ‘solution’. It uses four rational processes to approach problems:
Situation Analysis
Clarifies what happened in the problem situation
Problem Analysis
It answers ‘why it happened’, thereby identifying the underlying cause
Decision Analysis
It tells us how to act, thereby determining decision-making criteria
Potential Problem Analysis
It helps anticipate the results i.e., potential future problems or opportunities
Harappa’s Creating Solutions course is designed to help you get to the root cause of any problem. You’ll learn how to effectively analyze problems and ask the necessary questions to make sound decisions and judgments. The Synthesis Technique will help you examine results from your analysis—you can rely on this process to draw actionable insights. Be a meticulous problem-solver and stand out at work.
We use variations of root cause analysis in our daily lives. It can be best understood in the context of mental health. We get help by going to therapy because we want to resolve our unhealthy patterns and bring in fundamental changes to our behavior and thinking. Addressing the root cause of problems helps us lead healthier lifestyles in the long-run. This analogy is reflective of the fact that the root cause analysis can be a drawn-out but transformative process. So, don’t rush, analyze at your pace, and stay rooted!
Explore our Harappa Diaries section to know more about the topic related to the Solve habit such as Importance of Decision Making , Ethical Decision Making & FMEA in order to develop your problem-solving skills .
- RCA 101 – 5-Why Analysis (Free Training)
- RCA 201 – Basic Failure Analysis
- RCA 301 – PROACT® RCA Certification
- RCA 401 – RCA Train The Trainer
- Other Trainings
- 5 Whys Root Cause Analysis Template
- RCA Template
- Chronic Failure Calculator
A Beginners Guide To Root Cause Analysis (RCA) 2024
By Bob Latino
Updated: June 13, 2024
Reading Time: 4 minutes

WHAT IS ROOT CAUSE ANALYSIS (RCA)?
Basic steps of root cause analysis, rca methods, 4 key principles of root cause analysis, what rca tools do we recommend.
When issues arise within a company, there are a number of ways to problem solve. Root Cause Analysis (RCA) is an effective method to identify and solve problems in business by determining the underlying inefficiencies or imperfections and taking the necessary steps to address them to prevent the problem from arising again.
Root Cause Analysis (RCA) can be an effective tool for any business and is widely used in industries such as oil and gas, engineering, healthcare, aviation, and IT operations. RCA works backward in an attempt to zero in on the potentially minor errors that are causing or could cause major concerns.
Root cause analysis (RCA) is a systematic problem-solving technique used to identify the underlying causes of a particular issue or problem, rather than addressing only its symptoms. It involves a structured approach to investigating and understanding why something happened, with the goal of preventing its recurrence.
The term ‘RCA’ (Root Cause Analysis) is quite vague, misleading and easily misinterpreted by those who are not immersed in its use. It is a useless and counter-productive term because there is no universally accepted, standard RCA definition . Therefore, any process/tool someone is using to solve a problem is likely to be labelled as ‘RCA’.
It could be troubleshooting, brainstorming and/or some other more structured problem solving approaches such as 5-Whys, fishbone diagrams, causal factor trees and/or logic trees. Various regulatory agencies have their own such definitions, as do corporations and companies. However, when definitions differ between agencies, corporations and industries, it is hard to measure the effectiveness of ‘RCA’ across the board, because everyone considers whatever they are doing, as ‘RCA’.
These are the general steps involved in Root Cause Analysis. Keep in mind that specific methodologies and tools may vary depending on the context and industry.
- Define the Problem : The first step in Root Cause Analysis is to clearly define the problem or issue that needs to be addressed. It’s important to have a precise understanding of what went wrong and what the impact of the issue is.
- Identifying contributing factors
- Ranking factors by likelihood of causing the problem
- Classifying these factors into groups representing correlation, contribution, or “root cause” status
- Identify Root Causes : Once you have gathered data, you analyze it to identify the root causes of the problem. Root causes are the underlying factors that contributed to the issue. Techniques such as the “5 Whys” method or Fishbone Diagrams (Ishikawa Diagrams) are commonly used to uncover root causes.
- Develop and Implement Solutions : After identifying the root causes, the next step is to develop and implement solutions to address those root causes. These solutions should be designed to prevent the problem from recurring. It’s important to monitor the effectiveness of the solutions and make adjustments if necessary.
Additionally, incorporating lean six sigma green belt training and RCA can further enhance your ability to improve business processes and effectively implement Root Cause Analysis.
There are a variety of tools and methods to apply root cause analysis and the most effective tool may vary based on industry, company, the nature of the problem, etc. logic tree identifies the following common tools:
- 5 Whys is a popular tool that looks for the hidden cause by continuing to ask the question “why?” Though 5 is not always the magic number, it is often around the fifth “why” that the hidden cause is discovered.
- Fishbone is a cause and effect diagram that identifies multiple possible causes that could have led to the identified problem.
- A flowchart maps out all the steps of a process through different departments in an effect to identify where an error could have occurred.
- A Pareto chart is based on the premise that eighty percent of effects is caused by twenty percent of causes. It involves prioritizing possible causes based on likelihood of causing the identified problem.
The Washington State Department of Enterprise Services highlights four key principles involved in Root Cause Analysis:
1. There is usually more than one root cause for a problem
By making broad assumptions about what might be going wrong with business, an entire investigation can be derailed as you hone in one factor instead of investigating all potential contributing factors. RCA does not presume there is only one contributing factor but seeks to evaluate all factors that could be contributing to the systemic issue.
2. RCA is performed most effectively when accomplished through a systematic process with conclusions backed up by evidence
While it may be easy to identify a contributing factor and assume that is the root cause, RCA steers clear of a shallow investigation and looks at the entire system of “roots” as potential causes. RCA involves gathering quality evidence, not hearsay or unquantifiable data. RCA is not intended to be completed as a one man show, but rather a team effort that includes members from each potentially contributing department of the company.
3. The focus of the investigation should be “WHY the event occurred” not “WHO made the error.”
The goal of RCA is not to point fingers at an individual or department who made an error, but to identify systems that can be improved for overall the productivity of the company. RCA places the focus on why the event occurred by going step by step through each process leading up to the problem and evaluating all potential factors in play. The emphasis is on process improvement not on accusations.
4. Focusing on corrective measures of root causes is more effective than simply treating the symptoms of a problem or event
Unlike many problem solving methods that treat the symptom of a problem, Root Cause Analysis gets to the underlying “root” of the problem but investigation does not end at identification of root cause. Once one or more root causes are identified, corrective action is taken in order to prevent the problem from occurring again. RCA can also be used as a method in proactive management- identifying underlying errors before a problem has manifested.
While one can theoretically perform RCAs with sticky notes or on a blank excel sheet, simple tools designed for maximizing impact can be highly effective in taking your RCA game to the next level. EasyRCA is our software offering that is the culmination of 50+years experience in hands-on Reliability training and consulting. It is designed to get your organization to the root of the problem as quick as possible and without any training needed. EasyRCA is cloud-based, designed for team collaboration, and adaptable to multiple RCA methodologies to fit your company’s needs. Leadership can always view progress in real-time and teams can send off reports anytime with 1-Click professional formatting. Visit EasyRCA.com to learn more and book a Free Demo!
- Root Cause Analysis /
Recent Posts
How To Conduct Incident Analysis?
The Role of Artificial Intelligence in Reliability Engineering
Ultimate Guide to Swiss Cheese Model and Its Applications
5 Root Cause Analysis Examples That Shed Light on Complex Issues
advanced failure analysis
battling failure
PROACT® RCA System
root cause failure analysis
Root Cause Analysis Software
Our RCA software mobilizes your team to complete standardized RCA’s while giving you the enterprise-wide data you need to increase asset performance and keep your team safe.
Root Cause Analysis Training
[email protected]
Tel: 1 (800) 457-0645
Share article with friends:

RCA2: Improving Root Cause Analyses and Actions to Prevent Harm
This tool describes best practices for conducting a comprehensive Root Cause Analyses and Actions (RCA2) to improve patient safety by reducing medical errors, adverse events, and near misses; the Action Hierarchy tool helps identify which specific actions will have the strongest effect for successful and sustained system improvement.
- Root Cause Analyses and Actions (RCA2) event review process
- Action Hierarchy tool instructions, example, and template
Root cause analysis (RCA) is a process widely used by health professionals to learn how and why errors occurred, but there have been inconsistencies in the success of these initiatives.
To identify best practices around RCAs and develop guidelines to help health professionals standardize the process and improve the way they investigate medical errors, adverse events, and near misses, we have concentrated on the ultimate objective: preventing future harm. Prevention requires actions to be taken, and so we have renamed the process Root Cause Analyses and Actions, or RCA 2 (RCA “squared”) to emphasize this point.
The purpose of RCA 2 is to identify and implement sustainable systems-based improvements that make patient care safer in settings across the continuum of care. The approach is two-pronged:
- Identify methodologies and techniques that will lead to more effective and efficient RCA 2
- Provide tools to evaluate individual RCA 2 reviews so that significant flaws can be identified and remediated to achieve the ultimate objective of improving patient safety
The intent of an RCA 2 review is to identify system vulnerabilities so that they can be eliminated or mitigated; the review is not to be used to focus on or address individual performance, since individual performance is a symptom of larger systems-based issues.
After completing the RCA 2 investigation and analysis process, RCA 2 teams work to identify corrective actions to mitigate root causes of the adverse event. A tool such as the Action Hierarchy will assist clinical teams in identifying which actions will have the strongest effect for successful and sustained system improvement.
- Before filling out the templates, first save the PDF files to your computer. Then open and use that version of the tool. Otherwise, your changes will not be saved.
- IHI does not endorse any software or training for the RCA 2 process that is not directly provided by IHI.
How to Cite These Documents: RCA 2 : Improving Root Cause Analyses and Actions to Prevent Harm . Boston: National Patient Safety Foundation; 2015.
Patient Safety Essentials Toolkit: Action Hierarchy Tool . Boston: Institute for Healthcare Improvement; 2019. (Available at ihi.org)
Additional Information
- RCA 2 Frequently Asked Questions
- RCA 2 Endorsements
Related Content
- Patient Safety Essentials Toolkit
What Is RCA 2 ?
Download RCA2 and Action Hierarchy Tools
* Required fields
Related Resources
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Root cause analysis and medical error prevention.
Gunjan Singh ; Raj H. Patel ; Sarosh Vaqar ; Joshua Boster .
Affiliations
Last Update: February 12, 2024 .
- Continuing Education Activity
The term "medical error" encompasses diverse events that vary in magnitude and can potentially harm the patient. According to the 2019 World Health Organization (WHO) Patient Safety Factsheet, adverse events due to unsafe patient care are among the top 10 causes of death and disability worldwide. However, understanding that healthcare delivery involves multiple variables in a dynamic environment with many critical decisions made quickly is essential to finding the underlying causes of adverse events. Reducing medical errors requires a multifaceted approach at various levels of healthcare. In the event of a sentinel occurrence or adverse patient outcomes, a thorough evaluation is warranted to prevent such events. Root cause analysis provides a method of assessment for these situations so that a system-based intervention can be implemented rather than blaming individual clinicians. Upon completing this activity, healthcare professionals will gain a comprehensive understanding that root cause analysis (RCA) is a mandated process for healthcare institutions to mitigate future errors and promote patient safety. By acquiring proficiency in RCA application and methodology, healthcare professionals can effectively drive changes and improvements within the healthcare setting, resulting in enhanced patient care and a reduction in medical errors. The course also highlights the interprofessional team's role in performing this analysis to prevent medical errors and improve clinical outcomes.
- Implement effective root cause analysis of a sentinel event and strategies for prevention.
- Apply root cause analysis reporting standards in accordance with the Joint Commission requirements.
- Identify the indications for reporting sentinel events to the Joint Commission and the steps that should be taken following the occurrence of such incidents.
- Collaborate within an interprofessional team to prevent the most common types of clinical errors and improve clinical outcomes.
- Introduction
Medical error is an unfortunate reality of the healthcare industry and a continuously discussed topic due to its grave impact on patient care and outcomes. In a 1999 publication by the Institute of Medicine (IOM), it was highlighted that deaths resulting from medical error exceeded those attributed to motor vehicle accidents, breast cancer, or AIDS. [1] One study reported that approximately 400,000 hospitalized patients experience some preventable harm each year, while another estimated that >200,000 patient deaths annually were due to preventable medical errors. [2] [3] [4] Moreover, the reported cost of medical errors is wide-ranging, with some experts estimating healthcare costs of $20 billion each year, while others approximate costs of $35.7 to $45 billion annually from hospital-acquired infections alone. [2] [3] Subsequent reports that discuss potential etiologies of medical errors have blamed systemic issues. Others have focused attention on certain groups of patients that may be more vulnerable to medical error than others. [5] [6] Recently, the impact of medical errors on a patient's family members and healthcare professionals has been emphasized due to its effects on exacerbating burnout, poor work performance, mental health decline, and even suicidal ideation. [7] [8]
Though pinpointing the definitive cause of medical error in certain situations may be challenging, evaluating strategies that can be used to mitigate and prevent these adverse events from occurring in the first place is essential. One such method is root cause analysis, which has been shown to reduce clinical and surgical errors in various specialties by establishing a quality improvement framework. [9] This article will discuss the application of root cause analysis in medical error prevention and strategies for maintaining continuous quality improvement in the healthcare setting.
Sentinel Events and Root Cause Analysis
The Institute of Medicine defines a medical error as "the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim." [1] Recognizing the differences between medical malpractice and medical error is essential. An adverse event in a healthcare setting may be attributed to medical error and not meet the threshold of malpractice or negligence. Medical errors generally result from the improper execution of a plan or improper procedural planning. Thus, the complexity of the occurrence of a medical error can range widely and manifest in any aspect of patient care, from hospital admission to discharge, as well as the outpatient setting. Medical errors may occur without directly harming the patient; however, even in these instances, evaluating the cause of any medical error, whether or not the patient is harmed, and developing guidelines and strategies to prevent future occurrences is critical. [10] [11]
The Joint Commission defines a sentinel event as any unexpected adverse event "involving death, serious physical or psychological injury, or the risk thereof. The phrase 'or the risk thereof' includes any process variation for which a recurrence would carry a significant chance of a serious adverse outcome." Sentinel events indicate the need for an immediate investigation to discover the cause and develop corrective measures. Moreover, the Joint Commission reviews all sentinel events that have resulted in unexpected mortality, significant permanent harm, or severe, temporary harm requiring intervention to sustain life, which they require all member healthcare agencies to report. [12] [13] These events are not only debilitating to patients but can also impact the livelihood of healthcare providers. Sentinel events are unrelated to the patient's underlying medical condition but are attributable to improper medical intervention or improper technique. For instance, if a patient receives medication and experiences an anaphylactic reaction, clinicians must determine whether the reaction was due to the medication or failure to review the patient's allergies before administration. Thus, these cases must be critically reviewed to delineate whether or not the etiology of the error was preventable, which is often a challenging task.
Root cause analysis (RCA) is a process for identifying the causal factors of a medical error that may result in a sentinel event. A standardized RCA process is mandated by the Joint Commission to determine the cause of medical errors and thus allow healthcare institutions to develop strategies to mitigate future errors. [13] Despite broad adoption in the business, engineering, and industrial sectors, RCA use in the medical field has been limited. The RCA process aims not to assign individual blame but to identify lapses in system-level processes that can be restructured to prevent patient harm and reduce the likelihood of future sentinel events. Thus, identifying the root cause of a medical error can better direct the need for additional training and resources.
Applying Root Cause Analysis
For accreditation purposes, the Joint Commission requires that healthcare institutions have a comprehensive process for systematically analyzing sentinel events. The RCA process is one of the most commonly utilized tools for this purpose. Through the RCA process, healthcare institutions attempt to identify all the contributing factors that led to an adverse event. Essentially, RCA investigations continually question why a medical error occurred until all underlying deficiencies in a system are found. RCA emphasizes lapses in system-level processes rather than individual actions. Following a sentinel event, a designated RCA team must be assembled to review and identify necessary changes at the systematic level that can improve performance and reduce the likelihood of a repeat sentinel event. [14] Failure to perform an RCA within 45 days of a sentinel event may result in the healthcare institution being placed on an accreditation watch, which is public information. Repeat violations may result in an onsite review by the Joint Commission that may jeopardize accreditation. [15]
An RCA's initial step is forming an interprofessional team to investigate and define the problem. Typically, a designated process is implemented to communicate with senior leadership throughout the investigation, establish internal target dates, and meet Joint Commission deadlines. After identifying the problem, the team should evaluate systematic factors contributing to the error. Throughout the process, collecting data regarding the potential underlying causes is essential. The team should propose and implement immediate changes so that a repeat sentinel event does not occur during the RCA process. While developing these interventions, the team should evaluate the list of root causes, consider their interrelationships, and explore risk-reduction and process improvement strategies to prevent future errors at the systematic level. Furthermore, the team should discuss the proposed process modification with senior leadership and key stakeholders and determine if they are acceptable. There are various models used to guide RCA inquiries. One model is referred to as "The Swiss Cheese Model." According to this framework, errors occur due to failures on 4 primary levels, classified as unsafe acts, preconditions for unsafe acts, supervisory factors, and organizational influences that can allow patient injury when lined up. Therefore, RCA teams work to identify breakdowns on each of these levels that led to an adverse event. [16]
The Joint Commission has also created a framework with a series of 24 questions to organize an RCA and as a general template to prepare the report submitted to the Joint Commission. The 24-question guide considers various situational factors that may have contributed to a sentinel event. This includes examining the systematic process, human factors, equipment malfunctions, environmental factors, uncontrollable external factors, organizational factors, staffing and qualifications, contingency plans, performance expectations, communication issues, and technology. [13] With detailed consideration of each of these topics, an in-depth analysis of the cause of the sentinel event can occur. Communication is one factor examined in several of the 24 questions, including communication within organizational structure, conveying messages effectively and efficiently, and ensuring a proper communication system. Environmental factors should also be examined to determine if any situational issues were ongoing during the sentinel event that may have impacted the outcome. Moreover, staffing is another issue that should be examined during an RCA review to determine if the staff were appropriately qualified, competent, and portioned for their assigned duties. [17]
After discussion, evaluation, and analysis, corrective actions should be developed, identifying areas for targeted improvement. While utilizing the 24-question framework, causative etiologies should be considered to help determine areas that can be restructured to reduce risk. The root cause analysis should be clear and precise while providing appropriate depth and scope. The Joint Commission has identified a series of adverse events subject to their purview. Primarily, this would be a sentinel event that has resulted in death or permanent loss of function unrelated to any underlying medical conditions, including: [17]
- Patient suicide involving any patient who received care from a healthcare system, including the emergency department, within 72 hours following their discharge
- The unanticipated health issue of a full-term infant
- An infant discharged to the wrong family
- Abduction of any patient receiving care, treatment, or services
- Elopement of a patient within a healthcare setting, leading to harm
- Hemolytic transfusion reaction requiring administration of blood products
- Rape, assault, or homicide of anyone on healthcare premises
- Wrong patient, site, or procedure for any surgical procedures
- Unintended retention of a foreign body in a patient following surgery
- Severe neonatal hyperbilirubinemia
- Prolonged fluoroscopy with cumulative dose to the wrong body region
- Fire, flame, or unanticipated smoke, heat, or flashes during patient care
- Intrapartum maternal death
- Severe maternal morbidity
The finalized RCA report must follow a set standard to meet the Joint Commission's requirements, including:
- Participation of the organization's leadership and key stakeholders
- Thorough explanation of all findings
- Consideration of any relevant or applicable studies
- Internal accuracy and consistency, without contradictions or unanswered questions
Case Illustrations with Root Cause Analysis Interventions
The following cases illustrate various types of medical errors, the process of root cause analysis through which failures were identified, and how interventions were implemented in each situation to prevent similar errors in the future.
Case example 1
A 42-year-old primigravida woman at 34 weeks gestation was brought to the obstetric emergency department at midnight with complaints of severe headache, blurry vision, and right upper quadrant pain for the last 5 to 6 hours. She noted lower extremity edema and facial swelling that was gradually increasing. She has gestational hypertension and, 1 week ago, was prescribed labetalol 200 mg twice a day. On initial presentation, her blood pressure was 190/110 mm Hg on 2 separate occasions, 5 minutes apart. She had gained 2 kilograms since her last antenatal checkup in the clinic a week ago. The patient was diagnosed with severe preeclampsia. The senior obstetric resident ordered a loading dose of magnesium sulfate to prevent imminent seizure. The hospital protocol used an intravenous (IV) and intramuscular (IM) regimen where the patient received a 4 g IV bolus and a 10 g IM dose administered as 5 g in each buttock. The senior resident gave verbal orders for magnesium sulfate administration to the junior resident, who verbally communicated the order to the nurse.
The magnesium sulfate dosing regimen was complex, with multiple doses in different locations, and was incorrectly prepared by the nurse who felt rushed in an urgent situation. Because the chart displaying magnesium sulfate's preparation in the drug preparation room had faded, the nurse relied on her memory. As part of the protocol, the nurse recited the dosage to another nurse, who cross-checked it from a printed chart and noted the error in time. The senior resident also identified the error as the dose was communicated aloud, and the drug administration was stopped.
- Root cause analysis with corrective measures : A root cause analysis was performed, and measures were taken to avoid this problem. As the Institute of Safe Medication Practices recommended, magnesium sulfate was marked as a high-alert medication. Furthermore, premixed solutions prepared by the pharmacy for the bolus dosing were instituted instead of requiring nurses to mix this high-risk medication on the unit. The second nurse verification measure was retained, with the second nurse instructed to double-check all doses, pump settings, drug names, and concentrations before administration of any drugs. Moreover, the RCA recommended that all medication orders be provided in writing and entered in the electronic medical record using computerized provider order entry (CPOE) systems, regardless of the situation's urgency, to avoid dosing errors. The RCA team emphasized that verbal communication for medication administration should always be avoided. If verbal communication is necessary or unavoidable, the RCA recommended that the nurse taking the order read back the order given to the prescribing physician to minimize any prescribing errors.
Case example 2 (The name and date of birth used in this example are for illustrative purposes and do not represent an actual patient. Any similarities if noted, are purely coincidental.)
Anna Joy, date of birth October 30, 1991, was a primigravida at 30 weeks gestation admitted to a busy obstetric ward with complaints of intermittent cramping abdominal pain. She had come from Spain to visit her sister, who was living in Boston. The patient's ability to communicate in English was limited, preferring to speak Spanish. However, her husband and sister were fluent in English and assisted with translation throughout the history, exam, and admission. The patient was seen by an obstetrician who advised routine threatened preterm labor evaluation and observation.
Another patient, Ann Jay, date of birth September 30, 1991, was 34 weeks gestation and admitted to the same ward for gestational diabetes mellitus with hyperglycemia. A consulting endocrinologist advised glucose monitoring and insulin administration. The nurse taking care of the patient was given orders, performed a finger-stick blood glucose check, and informed the endocrinologist about the results over the phone. The endocrinologist advised 6 units of regular insulin before lunch. After being told by the nurse that the patient was feeling decreased fetal movement, the admitting obstetrician recommended ongoing observation and fetal kick counts.
The family members of the first patient, Anna Joy, informed the nurse that they were going to lunch. The morning shift nurse later required a half-day leave because of personal issues and quickly handed her patients to another nurse. The ward was busy and running at full capacity. The new nurse decided to give the insulin injection first as the patient was about to receive her lunch. She did not know that Anna Joy preferred communication in Spanish. The nurse asked a few questions and rushed through patient identification with the help of 2 unique patient identifiers. She administered the insulin injection to the first patient, only realizing later that the insulin was supposed to be given to the second patient, Ann Jay. The attending obstetrician and the endocrinologist were informed. They took the necessary measures and closely monitored the patient for the next few hours; however, no adverse effects were noted.
- Root cause analysis with corrective measures : A root cause analysis was performed, and measures were taken to avoid this problem. The RCA team noted that the nurse caring for both patients had worked in the hospital for 5 years and was recently transitioned to the obstetric ward. This had never happened to her before. The team recognized that the modern patient care delivery process relies on an interprofessional care team's efficient and effective integration. A clear, consistent, and standardized communication method between the team members contributes to safe patient care and minimizes the risk of adverse outcomes. The RCA team did not lay blame on the nurse involved. They instead instituted a standardized handoff platform and required all patient handoffs to occur using this format in the future. During shift change, the handoff between clinicians and nurses is pivotal in providing high-quality care. The aim should be to provide the oncoming team with up-to-date, accurate, and complete information. The RCA team outlined clinical education programs for nurses and clinicians to ensure high-quality and effective handoff occurs at every shift change and patient handoff. They also instituted mandatory use of hospital-based interpreters when communicating with patients who are not fluent in English. The hospital procedure for verifying patient identification using two unique patient identifiers, the name and the date of birth, was retained. However, an additional mandatory step of verifying the patient's identity using an arm-band barcode was instituted before every medication administration. They also highlighted patient charts and rooms when patients had similar names and dates of birth.
Case example 3
A 26-year-old primigravida at 39 weeks gestation with no associated high-risk factors was admitted to a busy labor and delivery floor with labor pains. The patient was managed according to routine labor protocol. When the patient had reached a cervical dilatation of 4 cm, the cardiotocograph showed prolonged fetal bradycardia lasting for 3.5 minutes, which did not resolve with conservative interventions. The patient was transferred to the operating room for an emergent cesarean section. The baby was delivered in good condition, with no intraoperative complications. Before closure, the operating obstetrician asked the scrub nurse to perform a surgical count. The scrub nurse reported a missing gauze piece from the surgical trolley. Therefore, the scrub and the floor nurses performed additional counts several times. A second on-call obstetrician was summoned to assist the primary surgeon in checking the surgical field for the missing gauze piece. The surgical gauze had a heat-bonded barium sulfate marker embedded in the fabric to help with x-ray identification. An intraoperative x-ray was obtained to evaluate for a retained sponge, and the results were negative. After discussing the case with the department chief, the abdomen was closed. Due to the associated delays, the operative time was significantly lengthened, totaling 2 hours and 30 minutes.
- Root cause analysis with corrective measures : An RCA of the event revealed inconsistent practices regarding the surgical count before initiating the procedure. Moreover, only the scrub nurse was responsible for performing this count. The RCA team determined that the surgical count is critical and must be performed in a standardized fashion to eliminate variation and minimize human error. They highlighted international standards that recommend standardizing the counting process and systematically tracking the instruments, gauze, and sponges in the sterile field. Subsequently, they instituted the World Health Organization's Surgical Safety Checklist as a mandatory step for all procedures, regardless of the urgency of the procedure. The team also recommended that the counting process be concurrently audible and visual, performed by the scrub nurse and the circulating nurse independently, and done before and after every procedure. They emphasized that the best practices for surgical count be followed regardless of the clinical situation.
Case example 4
A 25-year-old man presented for bilateral LASIK surgery at a same-day surgery center. The operating surgeon, a community-based surgeon not routinely operating at this facility, examined the patient, and informed consent was obtained preoperatively. The refractive error was -4 D for the right eye and – 5 D for the left eye. The plan was to remove the refractive error altogether. There was a timeout to ensure the correct patient and procedure. The LASIK procedure commenced by creating corneal flaps on both eyes, which was completed uneventfully. Then, the patient was adjusted on the operating microscope so that the first eye was directly under the excimer laser, and iris recognition was attempted before the laser-guided corneal power correction was performed. Though the machine did not recognize the iris pattern after 3 attempts, the surgeon decided to proceed. The technician thought this was rare as they had good iris recognition rates of >98% this month. However, he did not want to contradict the surgeon. Before the procedure, the circulating nurse noted that the patient's table was adjusted to the wrong side with the left eye under the laser instead of the right. She pressed the emergency stop button, and the treatment was terminated. After identifying the mistake, the surgeon and technician restarted the machine to treat the correct eyes in the correct sequence.
- Root cause analysis with corrective measures : Unlike unilateral procedures, bilateral procedures are especially challenging, particularly if the treatment varies between the 2 sides. An example is LASIK, where both eyes are typically corrected simultaneously, and there is no obvious pathology on the eye except for the refractive error. The correction is determined preoperatively, and the result is not immediately titrated. Therefore, the risk for wrong-site procedures is significant, given these ambiguities. To avoid these adverse events, the RCA team implemented a verification procedure where the optometrist, technician, and surgeon must verify each eye's refractive error before the procedure and after programming the laser. Some advanced laser machines have a built-in layer of defense where the iris pattern of the eye is uniquely identified via iris recognition, helping to determine the correct eye and enhance treatment protocol. Some treatments, however, do not include iris recognition, and therefore, the onus lies on the technicians, nurses, and surgeons to identify the appropriate eye correctly.
Case example 5
A community clinic treats approximately 110 patients daily. The clinic is run by 2 primary care physicians, with the assistance of 2 nurses and scribes. A 10-year-old boy was brought to the clinic by his parents due to a runny nose for the last 10 days. On examination, the primary care physician diagnosed allergic rhinitis and advised them to use over-the-counter cetirizine. One of the scribes had called in sick that day, so a secretary was assisting the physician. The physician advised the parents that cetirizine is an over-the-counter medication that could be obtained at their pharmacy of choice. After 2 days, the patient's mother returned to the clinic and reported that the child was lethargic. The clinic front desk staff told the mother they would convey this to the physician, who was very busy that day. The physician instructed the staff to inform the parents that somnolence was typical for children taking cetirizine and to keep the child at home for the next few days. The message was conveyed to the mother, who decided to take the child to another specialist as she was concerned by the sedation. The specialist noted that the child was taking a 10-mg cetirizine tablet twice a day, which is double the recommended amount.
- Root cause analysis with corrective measures : An RCA review at the primary clinic identified a typographical error in the patient instruction handout. Instead of 5 mg twice daily, the instructions had a dosage of 10 mg twice daily. Subsequently, the RCA recommended a verbal and written verification procedure be instituted with the prescribing physicians of all drugs and dosages transcribed by the scribes or office personnel. Moreover, the physician and staff were to read prescription and over-the-counter drug recommendations and doses to the patient or caregiver from the visit summary instructions to verify a match with the clinician's notes. The RCA also mandated a document review for all patient callbacks or return visits before communicating with a patient to avoid future errors.
Case example 6
All-Eyes Laser Center is a busy same-day ophthalmic laser center that performs multiple laser procedures daily but specializes in retinal and anterior segment lasers. A 60-year-old man, JM, suffered from chronic angle-closure glaucoma and had been advised to undergo a Yttrium-Aluminum-Garnett (YAG) laser iridotomy, which involves creating a small hole in the peripheral part of the iris to increase the aqueous flow between the anterior and the posterior chamber. This treatment is frequently performed to prevent an angle-closure attack and further glaucoma progression. This laser surgeon also does another laser procedure called a YAG capsulotomy in which the posterior capsule in a pseudophakic eye is lasered to create an opening to improve vision impaired by after-cataract posterior capsular opacity. The YAG laser device platform allows both procedures to be performed with one machine.
The day JM was scheduled for the YAG procedure was unusually busy at the laser center, and the surgeon was running behind schedule. There were 5 patients ahead of JM, and an approximately 2-hour delay was anticipated. With each patient, the typical practice before a YAG iridotomy procedure consisted of the nurse practitioner checking the patient history, confirming examination findings, and instilling 2% pilocarpine eye drops to cause constriction and ensure good exposure of the peripheral iris crypts. The laser surgeon would then perform the procedure, directing the laser to create a small iridotomy.
After JM was taken to the procedure room, a proper timeout was confirmed, including the correct eye and procedure. However, when the patient was positioned at the laser machine, the surgeon noticed that the pupil was dilated rather than constricted. The surgeon again verified the patient's tag and name and the correct procedure. Though the patient and the procedure were both determined to be correct, the surgeon believed attempting an iridotomy on a dilated pupil would be dangerous. Therefore, the procedure was not performed, and the patient was transferred out of the laser suite. The patient was informed of the error and instructed that he would be rescheduled for the correct procedure in a few days. The error was attributed to the nurse administering the wrong eye drop, secondary to high patient volume and practice inconsistencies.
- Root cause analysis with corrective measures : An RCA was performed, and measures were taken to avoid this problem in the future. Though this error did not harm the patient, the risk of the wrong procedure being performed was high. Therefore, the RCA team recommended segregating patients for YAG capsulotomy and YAG iridotomy to different seating areas that were clearly labeled. The 2 eye drops, tropicamide and pilocarpine, were kept in their respective areas, and the staff was not allowed to take them out from their designated area. A barcode-based verification was also instituted and used each time the drop was instilled. Many clinics utilize precautions for similar-sounding medications and patient names. However, in a clinic where multiple procedures with a relatively quick turnover are being performed, pre-procedure medications without designated patient areas have a significant risk of being mixed. Using the precautions such as those mentioned above can help reduce medication errors.
- Issues of Concern
The IOM identifies medical errors as a leading cause of death and injury. [1] According to the 2019 World Health Organization (WHO) Patient Safety Factsheet, adverse events due to unsafe patient care are among the top ten causes of death and disability worldwide. Preventable adverse events in the US cause an estimated 44,000 to 98,000 hospital deaths annually, which exceeds motor vehicle collision deaths. [1] Furthermore, in terms of health care, disability, and loss of productivity, medical errors are estimated to cost the community an additional 37.6 to 50 billion dollars. [1] The most severe consequences of medical errors are the adverse events patients and their families suffer. Therefore, utilizing RCA is critical to identify systemic flaws that led to a medical error so that corrective measures can be promptly implemented.
Types of Medical Errors
Healthcare professionals should be familiar with the different types of medical errors to understand better the adverse events that may be caused. Errors are not always due to human miscalculation or miscommunication, as outlined by the cases above. Some errors are inherent to clinical situations, such as patient falls in hospital settings and healthcare-associated infections. Common types of medical errors include surgical errors, diagnostic errors, medication errors, equipment failures, patient falls, hospital-acquired infections, and communication failures. [3] [18]
- Surgical errors : Errors in surgery have the highest risk of severe patient injury and death. Intraoperative errors are estimated to be the primary issue in 75% of malpractice cases involving surgeons. Surgical errors involving the wrong site, patient, or procedure should never occur. Investigations into the factors that led to these types of surgical errors have demonstrated that common causes include clinician factors (eg, feeling rushed, distractions, and fatigue), miscommunication, changing or inadequate staffing, organizational factors (eg, discarding specimens as waste and not labeling specimens), medical record issues, and cognitive errors. [19]
- Diagnostic errors : The National Academy of Medicine defines a diagnostic error as "the failure to establish an accurate and timely explanation of a patient's health problems or to communicate that explanation to the patient," therefore, delayed or missed diagnoses are considered errors as well. [20] According to the Joint Commission, diagnostic errors result in the death or injury of 40,000 to 80,000 patients annually. Diagnostic errors are most common in primary care solo practices due to workload, time constraints, and the inability to confer easily with colleagues. [21] Malignancies, surgical complications, and neurological, cardiac, and urological issues are the 5 conditions most frequently misdiagnosed. [22] [23] [24] According to studies, these conditions are frequently misdiagnosed secondary to knowledge gaps, resulting in deficient bedside assessment and clinical reasoning. Identifying these commonly misdiagnosed conditions is beneficial, as diagnostic errors are primarily cognitive rather than organization-based errors; therefore, clinicians can be forewarned of the potential challenges when caring for these patients. [25] In addition to a clinical knowledge deficiency, common contributing factors to diagnostic error include a clinician's fatigue, distraction, failure to consider differential diagnoses, neglect of diagnostic testing follow-up, and inadequate patient follow-up care. [11] [21]
- Medication errors : These errors are widely accepted as the most common and preventable cause of patient injury. [26] Because there are several components involved with patient medications (eg, prescribing, dispensing, dosing, and administering), errors can occur in any of those areas. The reported incidence of medication error-associated adverse events in acute hospitals is approximately 6.5 events per 100 admissions. [26] Medication errors before or after discharge from an acute care facility are the most easily overlooked or missed errors. [26]
- Equipment errors : Medical equipment design flaws, mishandling, user error, and malfunction are common causes of medical errors. Additionally, a significant number of medical devices have been implanted in patients (eg, pacemakers, defibrillators, and nerve and brain stimulators), which may malfunction and result in life-threatening complications. Equipment errors can be due to device differences between manufacturers, inadequate testing and maintenance, poor design, and poor maintenance. Errors involving tube and catheter connections (eg, using catheters for unintended purposes, running the wrong line through a pump, and misplacing feeding tubes into the lung) are also common. These adverse events can have life-threatening effects if a misconnection is not corrected early. [27] [28] To complicate the situation further, medications and food supplements are often delivered via these routes, and placement errors can result in administration or omission mistakes.
- Hospital-acquired infections : Healthcare-related infections are considered a failure of the system. As many as 1 in 20 hospitalized patients may acquire a healthcare-related infection, increasing complications and the length and cost of the hospital stay. Healthcare-related infections add close to $35 billion to the annual cost of healthcare in the United States. [29] Common causes of hospital-acquired infections include failure to practice basic hand hygiene and poor technique in placing indwelling urinary and vascular catheters. Subsequently, the most prevalent infections are catheter-associated urinary tract infections, surgical site infections, hospital-acquired pneumonia, central line-associated sepsis, and care-related skin and soft tissue infections. [29]
- Patient falls : Each year, over one-third of people older than 65 suffer a fall, with one-third of these causing injury. [30] In a healthcare setting, several factors may further increase the risk of falls, including blood loss medication side effects, post-anesthesia effects, decreased blood sugar, altered mental status, advanced age, mobility impairment, and inadequate staffing. [31]
- Communication errors : Optimal interprofessional communication, as well as with patients, is essential for patient care. Therefore, communication errors commonly result in adverse events. [32] Reasons for impaired communication include disruptive patient behavior, environmental distractions (eg, cell phones and pagers), cultural differences, hierarchy issues, personality differences, language barriers, and socioeconomic variables, such as education and literacy. [11] Additionally, errors in written communication, such as using nonstandard abbreviations, illegible handwriting, failure to question inappropriately written orders, and failure to complete correct specimen labeling, frequently occur. [11]
- Clinical Significance
RCA helps healthcare organizations study events that resulted in patient harm or undesired clinical outcomes and identify strategies to reduce further medical errors and improve patient safety. Clinician participation in root cause analysis is vital as these initiatives recognize and address essential patient care aspects. Through a review of data gathered by the Joint Commission, the most common categories of clinical error resulting in patient death, which can be prevented through root cause analysis, have been identified. These sentinel events, which account for a significant proportion of morbidity and mortality within the hospital setting, include: [13]
- Surgical errors
- Diagnostic errors
- Patient suicide
- Medication errors
- Equipment errors
- Hospital-acquired infections
- Patient falls
- Communication errors
Medical Error Prevention Measures
By identifying the deficiencies, failures, and risk factors that lead to an adverse event, corrective measures can be developed to prevent similar errors. Subsequently, individuals involved in every aspect of healthcare can help implement appropriate preventative strategies to reduce future medical errors and improve patient safety. [17] The following interventions are some strategies institutions have implemented to address these common systemic flaws.
Surgical Errors
Preventative measures for surgical errors have frequently consisted of adopting checklists, counting instruments, initiating antibiotic prophylaxis for deep vein thrombosis, and utilizing radio-frequency marked sponges. [3] Additionally, the performance of a surgical time-out has become a widespread strategy to reduce surgical errors. A time-out is a pause before a surgical procedure begins. The surgical team pauses and reviews the patient's identity, the consent form, the procedure being performed, and the correct anatomical structures and side involved, which should be marked on the patient's skin. If multiple procedures by separate surgical teams are planned, separate time-outs must be done. Surgeons and every surgical team member involved in the procedure must be present during the time-out, and any disagreement during the time-out should trigger an investigation by the surgical team until the discrepancy is resolved. [33]
Wrong-site surgery is a major cause of medical errors that can be mitigated through various preoperative safety checkpoints and has been the subject of a sentinel event alert by the Joint Commission. [13] [34] These errors have most commonly been noted in orthopedic surgeries. [35] Risk factors include several surgeons involved in surgical care or transfers to another surgeon for patient care, multiple procedures on a single patient, time constraint pressures, and unique circumstances requiring unusual or special positioning during a surgical procedure. [34] Wrong-site surgeries can easily be mitigated by ensuring proper preoperative measures, such as labeling the correct surgical site with an indelible pen or distinctively marking the nonsurgical site before the surgery. Intraoperative radiography can also assist in aiding the correct surgical site during the procedure.
Diagnostic Errors
Diagnostic errors such as misdiagnoses, delayed diagnostic test results, lack of staffing or physician availability, delays in order fulfillment, inadequate treatment, and delays within the emergency department can cause delays in medical treatment that may result in patient death and permanent injuries. Reducing diagnostic errors requires a comprehensive approach that implements various strategies due to the many factors that can lead to these errors. System-based safety checks and cognitive aids are often recommended as interventions to help prevent diagnostic errors. Cognitive aids include algorithms to help guide decision-making based on accepted guidelines, "trigger tools" within electronic health records that remind clinicians to consider differential diagnoses for commonly misdiagnosed conditions, and checklists to prevent the omission of critical steps. [11] [36] According to a 2015 New England Journal of Medicine article, trigger tools are essential in reducing this type of medical error. [36] Trigger tools are electronic algorithms that identify potential adverse events. This is accomplished by searching electronic health records and flagging specific occurrences. [36] The use of cognitive aids and trigger tools has been shown to decrease the rate of misdiagnoses in recent studies. [36] Addressing deficiencies through various other strategies (eg, device-based decision support, simulation-based training, and increased specialist utilization) may also help reduce diagnostic errors. [24] Though ingrained practice methods and physician overconfidence can attenuate the success of these interventions, fostering critical thinking and promoting "pause and reflect" methods have been found to help avert diagnostic errors, especially in cases with obscure clinical findings or unexpected clinical trajectories. [37] [25] Aside from encouraging critical thinking, opportunities for case discussions and second opinions should be made available for the treating providers. Healthcare facilities should also provide avenues for second opinions or interdisciplinary teams where cases can be discussed. [37] Other interventions to reduce diagnostic errors of commonly misdiagnosed conditions include simulation-based training, performance feedback, and encouraging the contributions of nurses, pharmacists, and other health professionals during patient care. [24]
Patient Suicide
Patient suicide is an unfortunate cause of death commonly seen in psychiatric care settings. [13] Several risk-reduction methods can be implemented for this adverse event, including ensuring a controlled environment free of hazardous materials, frequent patient observation, effective communication, adequate staffing in the facility, suicide assessment upon admission, regular psychiatric evaluation, and assessment for the presence of contraband.
Medication Errors
Medication administration errors are a common and avoidable adverse event that can occur at various patient care levels, involving many individuals in a multidisciplinary patient care team. [38] Barcode administration and handheld personal digital assistants increase medication administration safety by providing real-time patient information, medication profiles, laboratory values, drug information, and documentation. Moreover, electronic medication administration helps identify incorrect medications and orders that have been canceled or modified. However, circumventing barcode procedures decreases safety at the point of care. Automatic dispensing systems that quickly make drugs available to patients allow pharmacy clinicians to engage in other safety activities, such as medication reconciliation. Additionally, look-alike medications should be stored away from more dangerous medications. Hospitals can also standardize storage areas and avoid medication containers that have a similar appearance. Pharmacy clinicians should remove dangerous medications from floor stock and discard out-of-date drugs as a preventative measure. Other strategies include using color-coded intravenous lines, utilizing standard concentrations of vasoactive agents, labeling syringes immediately after preparation, and capitalizing the differences on the labels of medications with similar names. [11] [3]
Equipment Errors
Health professionals should be involved in setting and evaluating institutional, organizational, and public technology-related policies. Safety primarily can be improved by developing protocols for equipment maintenance, training, monitoring, and reporting adverse events related to technology. Additionally, clinicians should be educated in remaining vigilant despite clinical assistance by devices and able to manage equipment failure situations. [39] Unique connectors for anesthesia catheters and feeding tubes can be used to reduce the chances of tubing misconnections. [40] Furthermore, clinicians and support staff should always trace lines back to the origin before connecting or disconnecting devices or starting infusions and labeling high-risk catheters. [27] [28]
Hospital-acquired Infections
Changing the behaviors of healthcare team members is effective in reducing iatrogenic infections. Hand hygiene campaigns have been shown to decrease the number of nosocomial infection rates for various infections and should be universally endorsed. [41] Most healthcare facilities now employ specific protocols for minimizing central venous and urinary catheter use and using protective measures such as chlorhexidine for vascular catheter site care to reduce the incidence of healthcare-associated bloodstream infections, ventilator-associated pneumonia, and catheter-associated urinary tract infections. [3] Minimizing the duration of use of indwelling catheters has also effectively reduced the incidence of associated infections. [41] [3]
To decrease the risk of nosocomial infections, pharmacy-driven antibiotic stewardship programs should be regularly employed in all patients admitted to a healthcare facility. [42] Frequent skin assessment and evaluation by wound care teams with regular and focused nursing education and evidence-based treatments should be routinely employed to lower healthcare-associated pressure injuries. [43] The care of surgical sites should follow similar protocols, with some studies proposing chlorhexidine-impregnated dressings to decrease the incidence of surgical site infections. [3]
Patient Falls
Similarly, patient falls are a constant source of injury within healthcare facilities. Patients at high risk for falls should be identified, and appropriate safety precautions should be taken. Elderly patients tend to be prone to falls due to their age-related changes in vision or cardiovascular problems. Elderly patients also frequently have increased balance issues and muscle weakness over time, leading to ambulatory dysfunction. Having fall-prevention protocols in place, identifying potential high-risk areas within the home, and mitigating them through safety measures can improve patient safety and outcomes. [13]
Standardized protocols can reduce fall rates by ensuring a safe environment for risk-prone patients. Patient factors contributing to falls include advanced age, mobility impairment, and postsurgical effects. [31] Inadequate nurse staffing, an increased portion of staff made of new nurses, and increased shift hours are organizational factors that can lead to patient falls. [31] Implementing fall prevention protocols in hospitals and long-term care facilities has significantly reduced these errors. Furthermore, standardized fall risk assessments such as the Morse Fall Scale can decrease patient falls. [3] Institutional interventions such as staff education, patient mobility training with rehabilitation professionals, and nutritionist support have also been shown to reduce patient falls. [3] Other strategies include identifying patients at high risk for falls, providing patient safety companions, educating caregivers about fall prevention, and setting bed alarms and frequent safety rounds for all high-risk patients. [3]
Communication Errors
A courteous and respectful workplace where the interprofessional team collaborates promotes a safe work environment for all healthcare team members, families, and patients. Risk management committees and interprofessional task forces should work collaboratively on risk assessment and reduction. Joint education programs help providers and support staff learn roles and develop relationships to improve safety. The Joint Commission's Safety Goals require that for critical test results and verbal or telephone orders, a "read-back" verbatim to the practitioner by the person receiving and recording the result or order. The practitioner should then verbally acknowledge the accuracy of the order. [11]
Additionally, healthcare staff should avoid common errors in written communication, such as using nonstandard abbreviations, illegible handwriting, failure to question inappropriately written orders, and failure to complete correct specimen labeling. Therefore, staff should be encouraged to ask questions when uncertain and trained to double-check that the patient's name is spelled correctly and their correct date of birth is present. The Joint Commission requires healthcare professionals to use 2 or more patient identifiers when labeling, delivering, and maintaining specimens. Since this is a National Patient Safety Goal, The Joint Commission closely monitors healthcare institutions' adherence to this requirement as they prepare medications and transfusions and transfer patients from unit to unit. [11]
Clinicians should also follow well-communicated protocols that guide care and communication with patients. Age-associated hearing and cognitive decline increase the likelihood of communication errors regarding medications. Ensuring appropriate communication skills tailored to distinct patient groups is crucial in preventing such errors. Young children and infants are similarly prone to common medical errors due to the lack of direct participation in decision-making and patient care. Thus, specialized communication is needed to convey medical instructions to elderly and younger patients and their caregivers to ensure no lapses in communication. Providers should listen to patients' questions concerning how care is delivered. Concerns must be respected and accepted if care plans contradict established evidence-based medicine. Moreover, the Joint Commission has supported "speak up" initiatives, which encourage hospitals to inform patients about the importance of their contributions to the care they receive in preventing medical errors. To make patients active participants in avoiding medical errors, encourage patients to ask about unfamiliar tests, unplanned diagnostic tests, and medications and to verify the correct surgical site. [11] Additionally, skilled medical interpreters can be crucial in effectively communicating instructions and information to patients instead of family members, who may often be biased. Implementing standardized clinician-family communication at the patient bedside with family engagement and bidirectional communication also decreased the frequency of harmful medical errors and positively impacted the family experience. [44]
Communication errors during patient hand-offs can occur when incorrect information is passed to the receiving clinician, or pertinent information is omitted. [45] Several techniques developed to minimize errors when handing off patients include using electronic records and mnemonics (eg, situation, background, assessment, and recommendation [SBAR]) to address all pertinent information. [46] [47] The SBAR tool is considered a best-practice communication technique to deliver information in an organized and logical fashion during hand-off and critical patient care situations. [47] The US's National Academies of Sciences, Engineering, and Medicine also recommend that these hand-offs occur in real-time and allow the opportunity to ask and respond to questions regarding pertinent facts about patient care. [48] This principle should be used when discharging patients from the hospital as well. Clinicians should remember to perform a final bedside evaluation and review discharge instructions before sending any patient home, including giving the patient a thorough written follow-up plan, counseling on new medications, and instruction to return to the hospital or office for new or worsening symptoms.
- Enhancing Healthcare Team Outcomes
Medical errors are undeniably an essential cause of patient morbidity and mortality within the United States healthcare system. These errors are prevalent at rampant levels, and the consequences of such errors can severely impact the patient, family members, and clinicians. The interprofessional healthcare team plays an invaluable role in preventing medical errors; team effort is crucial in identifying strategies and solutions to reduce the burden of medical error on the healthcare system. Nurses, pharmacists, rehabilitation professionals, nutritionists, and physicians are integral to the patient care team and crucial in preventing medical errors. Practitioners who work in error-prone environments must recognize their roles as healthcare team members responsible for reducing unnecessary errors. [49] The interprofessional team members comprising the RCA team should include professionals from all disciplines to ensure an effective investigation and implementation of corrective measures.
Clinicians should not hesitate to provide their peers with assistance in recognizing particular sources of common medical errors to deliver better patient care. Equal accountability and responsibility of all healthcare team members are critical in preventing errors and providing superior patient safety. [1] Quality assurance teams should employ RCAs with every sentinal event, especially in situations when the identification of medical errors becomes difficult or complex due to many underlying factors. RCAs can help identify factors within the healthcare delivery process that may impede the ability to provide quality patient care. Given the preventable nature of most medical errors, a thorough RCA can improve patient safety and allow healthcare organizations to serve as a model for others.
Healthcare professionals should be aware of common medical error sources and work as a team to identify possible risks when they become apparent. Doing so will increase the quality and efficiency of the healthcare industry and patient trust in the healthcare system. When an RCA is performed, the cooperation of all healthcare team members and clinicians involved in patient care is critical to understanding the underlying source of a medical error and identifying future strategies to mitigate such errors and improve patient outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Gunjan Singh declares no relevant financial relationships with ineligible companies.
Disclosure: Raj Patel declares no relevant financial relationships with ineligible companies.
Disclosure: Sarosh Vaqar declares no relevant financial relationships with ineligible companies.
Disclosure: Joshua Boster declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Singh G, Patel RH, Vaqar S, et al. Root Cause Analysis and Medical Error Prevention. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Medical Error Reduction and Prevention. [StatPearls. 2024] Medical Error Reduction and Prevention. Rodziewicz TL, Houseman B, Vaqar S, Hipskind JE. StatPearls. 2024 Jan
- Prevention of Surgical Errors. [StatPearls. 2024] Prevention of Surgical Errors. Santos G, Jones MW. StatPearls. 2024 Jan
- Medication Dispensing Errors and Prevention. [StatPearls. 2024] Medication Dispensing Errors and Prevention. Tariq RA, Vashisht R, Sinha A, Scherbak Y. StatPearls. 2024 Jan
- Review Improving safety for children with cardiac disease. [Cardiol Young. 2007] Review Improving safety for children with cardiac disease. Thiagarajan RR, Bird GL, Harrington K, Charpie JR, Ohye RC, Steven JM, Epstein M, Laussen PC. Cardiol Young. 2007 Sep; 17 Suppl 2:127-32.
- Review Tuberculosis. [Major Infectious Diseases. 2017] Review Tuberculosis. Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, Knight G, Murray M, Nardell E, Rubin E, et al. Major Infectious Diseases. 2017 Nov 3
Recent Activity
- Root Cause Analysis and Medical Error Prevention - StatPearls Root Cause Analysis and Medical Error Prevention - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Artificial Intelligence
- Generative AI
- Cloud Computing
- Data Management
- Emerging Technology
- Technology Industry
- Software Development
- Microsoft .NET
- Development Tools
- Open Source
- Programming Languages
- Enterprise Buyer’s Guides
- Newsletters
- Foundry Careers
- Terms of Service
- Privacy Policy
- Cookie Policy
- Copyright Notice
- Member Preferences
- About AdChoices
- E-commerce Affiliate Relationships
- Your California Privacy Rights
Our Network
- Computerworld
- Network World

4 steps to improve root cause analysis
Teams that follow observability standards, use monitoring tools, and foster a culture of collaboration can more quickly discover the root cause of system outages and performance issues..

When there’s a major systems outage or performance issue, IT teams come to the rescue to restore services as quickly as possible. Some IT organizations follow IT service management (ITSM) incident management practices to restore service, then follow problem management procedures to perform root cause analysis (RCA). More advanced organizations may employ site reliability engineers (SREs) involved in incident and problem management, but their primary responsibility is to drive more proactive steps to reduce error rates and improve service level objectives .
While much of IT operations tends to focus on major incidents like outages, disruptive performance issues, and security attacks, one of the more difficult challenges is finding the root cause behind sporadic, needle-in-a-haystack issues. These issues are infrequent, impact a small subset of users, or last for a very short duration. However, they can be very damaging to the business if they occur during critical operations performed by important end users.
Here are some examples:
- A user creates a complex website search or database query that hoards system resources and bottlenecks all other searching activities.
- A transaction locks system resources and only creates a performance issue when multiple users perform the same transaction simultaneously.
- A faulty cable, network card, or other device creates packet loss, but the impact is only felt by end users during peak usage periods.
- A database backup procedure’s duration increases as data grows, creating performance issues only for a subset of end users.
- A third-party service has slower-than-usual response times and degrades performance for dependent applications.
“Narrowing down difficult application performance issues requires a functioning debugging and feedback loop,” says Liz Fong-Jones, field CTO of Honeycomb . “Simple, quick issues often turn up in a spike in a single pre-aggregated query on a dashboard, but any issue more complicated than that is, by definition, an “unknown unknown” that was not previously seen or anticipated by the developer at the time they wrote the code.”
Finding the root cause of sporadic performance issues
As a developer in my younger days and later as a CIO, I’ve experienced many needle-in-the-haystack issues, and finding the root cause can be time-consuming and error-prone.
Sometimes, the challenge is sorting out the root cause from too much data, a problem AIops platforms can help address. Other times, there’s missing data, data quality issues, or data sets that need joining. Geoff Hixon, VP of solutions engineering at Lakeside Software , says, “Application performance issues aren’t always easy to find and fix, especially with gaps in data that can cause blind spots of the true root cause.”
How to perform root cause analysis (RCA)
What is needed is a process SREs, developers, and IT operational engineers can follow to perform RCA on issues that are harder to find. I propose four steps:
- Manage observability as a product
- Plan for top-down and bottom-up analysis
- Determine whether it’s a network issue
- Collaborate and triangulate on root causes
Step 1: Manage observability as a product
In my book, Digital Trailblazer , I tell several stories about fixing performance issues using observability. “It’s easy for people to chase the white rabbits and take other wrong turns, and observability data should help guide teams on the optimal focus areas.”
A devops best practice is to improve the observability of microservices , data pipelines, applications, and other in-house developed software. The challenge for many organizations is creating and improving data standards so that consistency improves ease of use when RCA is needed.
Nick Heudecker, senior director of market strategy and competitive intelligence at Cribl , recommends taking standardization one step further and treating application logs as a data product designed to be consumed by IT operations. “The most important factor in identifying application performance issues is ensuring the telemetry coming from apps is usable by downstream systems. This means structuring logs, enriching them with the right context, and delivering them to relevant platforms. Sounds simple, but the challenge is that the developers producing the logs often aren’t the people using them on the operations side.”
Standardizing observability data is one way to productize observability and simplify it for operational needs. Other best practices for devops observability include consulting with risk management on sensitive data and data retention policies. Devops teams should also take steps to educate SREs and people working in the network and security operation centers (NOCs and SOCs) to connect what the software does with how observability data is represented in logfiles and other repositories.
For large organizations developing many applications and microservices, observability standards must be coupled with automation, analytics tools, and models to make root cause analysis easier.
“A shift to a more targeted, real-time data analysis mindset in a company’s observability practice empowers engineers to proactively query the data and gain the insights needed to solve the most perplexing application performance issues,” says Asaf Yigal, co-founder and CTO of Logz.io . “To get to the root cause and resolve critical performance issues of modern microservice-heavy systems, a more efficient solution that cuts through the data using automation and enables proactive rather than reactive response is required.”
It’s important to have a continuous improvement mindset and incremental release strategy to observability standards. As NOCs, SOCs, and SREs encounter new issues, devops teams should use the feedback to improve data collection.
Step 2: Plan for top-down and bottom-up analysis
It’s relatively easy to find a slow query with basic database logfiles. Identifying root causes becomes more complex when query performance only degrades when the database is under load and multiple queries compete for the same system resources.
Grant Fritchey, devops advocate at Redgate Software , shares an example of a query that was running fast, about 6ms on average. “From a performance measurement standpoint, it was an unimportant query, until you saw the execution counts and realized that the query was called thousands of times per minute. Even at 6ms, it wasn’t running fast enough. This underscores the need for integrating observability and database monitoring tools to achieve a holistic and nuanced understanding of system performance.”
Effective RCA requires monitoring tools to do more than basic alerting of outages or major performance. Ops and SREs need indicators when performance is outside the norm and tools for top-down analytics to drill into suspect transactions and activities. Tools should also help identify performance outliers, especially for high-volume and poor-performance activities. The better tools also help isolate end-user experiences, so when there’s a customer support call about a problem, operations have tools to perform an RCA for that user.
Step 3: Determine whether it’s a network issue
It’s easier for devops teams to point to problems in the network and infrastructure as the root cause of a performance issue, especially when these are the responsibility of a vendor or another department. That knee-jerk response was a significant problem before organizations adapted devops culture and recognized that agility and operational resiliency are everyone’s responsibility.
“The villain when there are application performance issues is almost always the network, and it’s always the first thing we blame, but also the hardest thing to prove,” says Nicolas Vibert of Isovalent . “Cloud-native and the multiple layers of network virtualization and abstraction caused by containerization make it even harder to correlate the network as the root cause issue.”
Identifying and resolving complex network issues can be more challenging when building microservices, applications that connect to third-party systems, IoT data streams, and other real-time distributed systems. This complexity means that IT ops need to monitor networks, correlate them to application performance issues, and perform network RCAs more efficiently.
“Integrated packet monitoring across virtualized environments over north-south and east-west traffic paths provides consistent, real-time insights into traffic and application performance,” says Eileen Haggerty, AVP of product and solutions marketing at NETSCOUT . “But every domain and location must have the same analytics, intelligence, and visibility level, no matter where workloads, apps, and services are running. A consistent measurement approach across every hosting environment enables easier and faster determination of the root cause and location of performance issues for applications across any network infrastructure.“
Step 4: Collaborate and triangulate on root causes
Two other recommendations focus on how teams collaborate to resolve incidents and perform root cause analysis. I’ve led more than my fair share of bridge calls and rooms to find and fix issues, which can be a necessary evil during a major outage. However, these approaches are far less effective when solving sporadic performance issues that require correlating data from multiple tools and observability data sources. Many of these issues require a cross-disciplinary team to collaborate, share knowledge, and work together efficiently when an RCA is needed.
“I have observed a notable absence of application documentation and limited communication between teams in many larger and well-established organizations, says Chris Hendrich, associate CTO at SADA . “Breaking down these disjointed silos can help companies improve their ability to conduct root cause analysis.”
The second speaks to how teams search for root causes. Fong-Jones of Honeycomb says, “It’s not necessary to leap directly to the needle in the haystack, only to be able to narrow down parts of the haystack that the needle is or isn’t in until you find the needle. But, tools can help generate questions that will help you filter the haystack.”
All IT organizations run into performance issues that are hard to solve. Teams that collaborate, share information, create observability standards, and develop expertise in using monitoring tools can lower the stress, reduce the time, and improve the accuracy of their RCAs.
Related content
How to use fastendpoints in asp.net core, microsoft updates its serverless azure functions, microsoft moves forward with c# 13, offering overload resolution, amazon bedrock updated with contextual grounding, rag connectors.

Isaac Sacolick, President of StarCIO , a digital transformation learning company, guides leaders on adopting the practices needed to lead transformational change in their organizations. He is the author of Digital Trailblazer and the Amazon bestseller Driving Digital and speaks about agile planning , devops, data science, product management, and other digital transformation best practices. Sacolick is a recognized top social CIO, a digital transformation influencer, and has over 900 articles published at InfoWorld, CIO.com, his blog Social, Agile, and Transformation , and other sites.
The opinions expressed in this blog are those of Isaac Sacolick and do not necessarily represent those of IDG Communications, Inc., its parent, subsidiary or affiliated companies.
More from this author
7 steps to improve analytics for data-driven organizations, how to choose a data analytics and machine learning platform, advanced ci/cd: 6 steps to better ci/cd pipelines, 12 principles for improving devsecops, 10 principles for creating a great developer experience, 7 innovative ways to use low-code tools and platforms, how to test large language models, what is agile methodology modern software development explained, most popular authors.

Show me more
Enhancing your cyber defense with wazuh threat intelligence integrations.

How platform teams build better, faster, stronger enterprises

Progressive web app essentials: Background syncing

How to use dbm to stash data quickly in Python

How to auto-generate Python type hints with Monkeytype

How to make HTML GUIs in Python with NiceGUI

Sponsored Links
- Get Cisco UCS X-Series Chassis and Fabric Interconnects offer.
Free lower 48 U.S. Shipping on orders over $60 x
Item added to your cart
What is root cause analysis a complete guide.

What is Root Cause Analysis?
Root Cause Analysis (RCA) is a problem-solving method aimed at identifying the primary cause of a problem. Unlike other approaches that might focus on addressing immediate symptoms, RCA digs deeper to uncover the underlying issues that lead to a problem. This in-depth analysis ensures that solutions are more effective and lasting, reducing the likelihood of the problem recurring. This analytical approach encompasses a variety of methods, tools, and techniques designed to uncover the fundamental reasons for a problem or incident. With the primary goal of determining what happened, why it happened, and how to prevent it, root cause analysis is a widely used tool to improve safety, efficiency, and quality in various industries.
Principles of Root Cause Analysis
The root cause analysis method is built on 6 key principles. This includes:
- Focus on the Root Cause, Not Symptoms - believes that while symptoms are often the most visible aspects of a problem, they are merely the manifestations of deeper issues. RCA aims to move beyond these surface-level symptoms to find the underlying cause.
- Systematic Approach - follows a structured process that ensures a thorough investigation. This typically includes defining the problem, gathering data, identifying possible causes, and determining the root cause.
- Data-driven - involves collecting accurate information related to the problem, such as time of occurrence, conditions present at the time, and the sequence of events. Data analysis helps in identifying patterns and correlations that might point to the root cause.
- Involvement of Stakeholder - necessitates the direct involvement of stakeholders impacted by or have knowledge of the problem to provide valuable insights and a more comprehensive understanding of the issue.
- Prevention-Focused - aims to prevent future occurrence of the problem by addressing the root cause and implementing solutions aimed at eliminating the possibility of recurrence.
- Continuous Improvement - establishes that RCA is not a one-time activity but part of an ongoing process of continuous improvement .
What is the Goal of Root Cause Analysis?
The primary objective of Root Cause Analysis (RCA) is to identify the fundamental causes of problems or incidents to prevent their recurrence, leading to several key outcomes that significantly benefit organizations. By identifying root causes, RCA helps organizations understand underlying issues, allowing them to develop targeted, effective, and sustainable solutions. This thorough approach also enhances processes and systems by uncovering and addressing systemic weaknesses, which can improve overall efficiency, quality, and safety. RCA's proactive approach prevents future problems, saving time, resources, and effort by reducing the likelihood of recurring issues. Additionally, RCA provides a structured framework for problem-solving. This framework involves systematic data collection and analysis, helping organizations make better decisions regarding process improvements, resource allocation, and strategic planning. Ultimately, RCA fosters a culture of continuous improvement and proactive problem prevention within organizations.
Challenges and Limitations to Root Cause Investigation
Although root cause analysis is a powerful tool for identifying the underlying causes of problems and is key to implementing effective solutions, this approach comes with some challenges and limitations: Time-Consuming Conducting RCA can be time-consuming, especially for complex problems that require extensive data collection and process analysis . The thorough investigation can take considerable time and effort, which might delay the implementation of solutions. Resource Intensive RCA often requires significant resources, including skilled personnel, tools, and time. Small organizations or those with limited resources might find it challenging to conduct comprehensive RCA. Additionally, involving multiple stakeholders and experts can add to the resource requirements. Requires Accurate Data The effectiveness of RCA relies heavily on the availability and accuracy of data. Incomplete or inaccurate data can lead to incorrect conclusions and ineffective solutions. Organizations need to ensure proper data collection and management practices to support RCA. Potential for Misidentification If not conducted properly, there is a risk of misidentifying the root cause, which can lead to ineffective solutions and wasted resources. Proper training and expertise are required to conduct RCA effectively and avoid such pitfalls. Resistance to Change Implementing solutions based on RCA findings may require changes in processes or behaviors, which can face resistance from employees or stakeholders. Overcoming this resistance requires effective communication, change management strategies, and sometimes cultural shifts within the organization.
Root Cause Analysis Report: Step-by-Step Guide

Root cause analysis follows a structured approach to accurately identify underlying causes problems to prevent recurrence. Here’s a detailed guide on the steps involved in conducting an effective RCA: 1. Define the Problem The first and most crucial step in RCA is to clearly define the problem that the analysis is trying to address. A well-defined problem statement provides a clear understanding of the issue and sets the direction for the analysis. This involves describing the problem in detail, specifying its nature, what happened, where and when it occurred, as well as its impact on the business and its operations. This step also takes into account the symptoms that indicate the presence of the problem, such as specific failures or incidents. 2. Collect Data Gathering accurate and relevant data is essential for understanding the problem and identifying potential causes. It is a key component of the investigation process where the incident or problem is analyzed. Data collection might include machine maintenance schedules, operator logs, production output records, and recent changes in the manufacturing process. This step involves:
- Quantitative Data: Collect numerical data such as production logs, maintenance records, and performance metrics.
- Qualitative Data: Gather descriptive information such as operator observations, incident reports, and interviews with those involved.
3. Identify Possible Causes Identifying possible causes is a critical step in Root Cause Analysis (RCA), as it helps to uncover the various factors that might contribute to the problem. This step involves a systematic exploration of potential causes using specific tools and techniques such as brainstorming with a diverse group of stakeholders, the fishbone diagram, or the 5 Whys technique. 4. Determine the Root Cause Determining the root cause involves analyzing the possible causes identified in the previous step to pinpoint the fundamental issue. This step is crucial for developing targeted solutions that address the core problem. The process typically involves:
- Cause-and-Effect Analysis - This assesses the relationship between potential causes and the problem. This analysis helps in understanding how different factors interact and contribute to the issue. Tools like the Fishbone Diagram and 5 Whys technique can be instrumental in this analysis.
- Evaluating Evidence - Reviewing the evidence collected during data collection helps in validating the potential causes. This involves examining data points, cross-referencing information, and looking for patterns or correlations that support the identification of the root cause.
- Validating the Root Cause - Once the root cause is identified, it is essential to validate it by considering all the evidence and ensuring that it directly leads to the problem. This validation ensures that the analysis is accurate and that the solutions developed will effectively address the issue.
5. Develop and Implement Solutions Once the root cause of the problem has been identified, the next step is to develop and implement solutions that address this root cause. This step involves a series of actions aimed at ensuring that the problem does not recur and that the underlying issues are effectively resolved. The first part of this step is to brainstorm and develop solutions specifically aimed at addressing the root cause. These solutions should be practical, feasible, and effective. It is important to consider the resources available and the potential impact of the solutions. After developing the solutions, the next step is to create a detailed implementation plan. This plan should outline the specific actions needed to implement the solutions, assign responsibilities, and set timelines. The plan should also include measurable objectives to track the progress and effectiveness of the implemented solutions. With the implementation plan in place, the next step is to execute the plan. This involves carrying out the tasks as outlined, ensuring that each action is completed as scheduled. It is important to maintain clear communication and coordination among all involved parties to ensure smooth execution. 6. Verify Effectiveness After implementing the solutions, it is crucial to verify their effectiveness to ensure that the problem has been resolved and that the solutions are working as intended. This step involves monitoring, evaluating, and adjusting the solutions as necessary. Continuous monitoring is essential to determine whether the implemented solutions are effective. This involves collecting data and observing the situation to see if the problem has been resolved and if any new issues have arisen. Additionally, analyze the data collected during the monitoring phase to evaluate the effectiveness of the solutions. Compare the current situation to the baseline data collected before the implementation to determine if there have been improvements. If needed, implement changes and adjustments that would refine the solutions or address additional root causes.
7 Different Root Cause Analysis Tools & Techniques

Root Cause Analysis (RCA) employs various tools and techniques to identify the underlying causes of problems. Here is a closer look at the most commonly used RCA tools and methodologies:
Fishbone Root Cause Analysis
The Fishbone Diagram , also known as the Ishikawa Diagram or cause-and-effect diagram, is a visual tool used to systematically identify potential causes of a problem and organize them into categories. This method helps teams brainstorm and visually map out the various factors contributing to a specific issue, making it easier to see the relationships between causes and effects. The diagram resembles a fishbone, with the problem or effect at the "head" and potential causes categorized into major groups branching off the "spine." Common categories include People, Processes, Equipment, Materials, Environment, and Management. Key Features:
- Comprehensive View: Provides a holistic view of the problem by considering all possible causes.
- Visual Clarity: Offers a clear and organized way to visualize complex relationships between causes and effects.
- Facilitates Team Collaboration: Encourages collaborative brainstorming and involvement from multiple stakeholders, ensuring diverse perspectives are considered.
5 Whys Root Cause Analysis
The 5 Whys technique is a simple yet powerful tool used in Root Cause Analysis to identify the underlying cause of a problem. It involves asking "why" multiple times (typically five) to delve deeper into the cause of an issue until the fundamental cause is identified. The process begins with stating the problem clearly. Then, by repeatedly asking "why" and answering the question, the analysis drills down to the root cause. Each answer forms the basis for the next "why" question, helping to peel away layers of symptoms to reach the core issue. Key Features:
- Simplicity: Easy to implement and understand, requiring no complex tools or extensive training.
- Effectiveness: Helps to quickly identify the root cause of a problem by focusing on direct cause-and-effect relationships.
- Engagement: Encourages participation and input from team members, fostering a collaborative approach to problem-solving.
PROACT Root Cause Analysis
PROACT is a structured root cause investigation methodology designed to systematically identify and address the underlying causes of problems. PROACT stands for Problem definition, Root cause identification, Option generation and selection, Action plan implementation, and Track effectiveness. Key Features:
- Structured Approach: Provides a clear, step-by-step process for conducting RCA, ensuring thorough analysis and effective solutions.
- Comprehensive: Covers all aspects of problem-solving from definition to tracking effectiveness, leading to sustainable improvements.
- Focus on Implementation: Emphasizes the importance of implementing and monitoring solutions, ensuring that corrective actions are effective and long-lasting.
Fault Tree Analysis (FTA)
Fault Tree Analysis (FTA) is a top-down, deductive failure analysis technique used to analyze the probability of specific system failures. It begins with an undesired event (the top event) and works backward to identify all possible causes (faults) using logic diagrams. Key Features:
- Visual Representation: Provides a clear and visual representation of the relationships between different causes and the top event, making complex interactions easier to understand.
- Systematic Analysis: Offers a systematic approach to identifying and analyzing potential failure paths, ensuring thorough investigation.
- Prioritization: Helps prioritize causes based on their contribution to the top event, allowing for focused and effective mitigation measures.
Failure Mode and Effect Analysis (FMEA)
Failure Mode and Effect Analysis (FMEA) is a systematic method for evaluating processes to identify where and how they might fail and assessing the impact of different failures. It helps prioritize which potential failures should be addressed first based on their severity, occurrence, and detectability. This approach involves identifying potential failure modes, analyzing effects and causes of each failure mode to identify potential causes, evaluating the associated risks for each identified failure mode, calculating the risk priority number, and developing and implementing action plans. Key Features:
- Proactive Approach: Identifies potential failures before they occur, allowing for preventive measures to be implemented.
- Comprehensive Analysis: Provides a detailed and systematic evaluation of potential failure modes and their effects, leading to a thorough understanding of risks.
- Prioritization of Risks: Helps prioritize risks based on their severity, occurrence, and detectability, ensuring that the most critical issues are addressed first.
Scatter Plot Diagram
A Scatter Plot Diagram is a graphical representation that can be used in root cause investigation to identify and visualize the relationship between two variables. By plotting data points on a graph, it helps to detect correlations, patterns, and trends that may indicate potential causes of a problem. Data points representing pairs of variables are plotted on a graph. The pattern of the points can reveal relationships, such as positive or negative correlations, or lack thereof. Key Features:
- Identifies Relationships: Helps to identify and visualize correlations between two variables, making it easier to understand their impact on the problem.
- Data-Driven Analysis: Provides a factual basis for analysis, allowing for more objective decision-making.
- Detects Patterns: Can reveal trends and patterns that might not be immediately obvious, helping to pinpoint underlying causes.
Affinity Diagram
An Affinity Diagram is a root cause analysis tool used to organize a large number of ideas or pieces of information into logical groupings based on their natural relationships. This technique is particularly useful during brainstorming sessions to help categorize and prioritize potential causes of a problem. Ideas generated during brainstorming are written on cards or sticky notes. These are then grouped based on their similarities or affinities. Each group is given a heading that describes the common theme. Key Features:
- Organizes Information: Helps to organize large amounts of information into manageable and meaningful categories.
- Encourages Collaboration: Promotes team collaboration and input, ensuring that all relevant ideas are considered.
- Prioritizes Issues: Makes it easier to prioritize issues by grouping similar ideas together, helping to focus on the most critical areas.
These tools allow organizations to systematically identify root causes. Each tool offers a unique approach to problem-solving, making it important to select the appropriate technique based on the specific context and nature of the problem.
What are KPI in root cause analysis?
Key Performance Indicators (KPIs) in Root Cause Analysis are metrics used to measure the effectiveness and efficiency of the RCA process. Common KPIs include the number of incidents analyzed, time taken to complete RCA, recurrence rate of issues, and the success rate of implemented solutions.
How to prioritize root causes?
Root causes can be prioritized based on their impact, frequency, and feasibility of addressing them. Using tools like the Risk Priority Number (RPN) in Failure Mode and Effect Analysis (FMEA), or assessing factors such as severity, occurrence, and detectability, helps determine which root causes should be addressed first.
Who is responsible for RCA quality?
The responsibility for RCA quality typically lies with the RCA team leader or facilitator, who ensures that the analysis is thorough, accurate, and objective. Additionally, all team members, including subject matter experts and stakeholders, contribute to maintaining high-quality standards throughout the RCA process.
What is RCA in QMS?
In Quality Management Systems (QMS), Root Cause Analysis (RCA) is a critical process used to investigate and resolve non-conformities, defects, and quality issues. It helps identify the underlying causes of problems and implement corrective actions to prevent recurrence, thereby improving overall quality and compliance.
How to identify root causes?
Root causes can be identified using various tools and techniques, such as the 5 Whys, Fishbone Diagram (Ishikawa), Fault Tree Analysis (FTA), Failure Mode and Effect Analysis (FMEA), and the Apollo Method. These methods help systematically explore and analyze potential causes to uncover the fundamental issues behind a problem. TRADESAFE is an established American-based and owned company trusted by thousands for industry safety supplies and equipment. We offer Lockout Tagout products, eye wash stations , workplace signs , and more; all precision-engineered to enhance and ensure workplace safety.
The material provided in this article is for general information purposes only. It is not intended to replace professional/legal advice or substitute government regulations, industry standards, or other requirements specific to any business/activity. While we made sure to provide accurate and reliable information, we make no representation that the details or sources are up-to-date, complete or remain available. Readers should consult with an industrial safety expert, qualified professional, or attorney for any specific concerns and questions.
ENSURE SAFETY WITH PREMIUM SOLUTIONS
Author: steven stogner.
Steven Stogner is a seasoned safety professional with 14 years in sectors like heavy industrial construction and petrochemical. He is a Certified Safety Professional, skilled in incident analysis and root cause methodologies. Holding a BS in Industrial Technology from Southeastern Louisiana University, he is a recognized contributor to safety publications. At TRADESAFE , Steven enhances product development and supports the creation of key safety resources, strengthening the brand’s commitment to workplace safety.
Your cart (0)
- Choosing a selection results in a full page refresh.

IMAGES
VIDEO
COMMENTS
Conducting a root cause analysis can help schools and districts strengthen their school improvement planning efforts in a variety of ways. For schools and districts that have already conducted a needs assessment, engaging in a root cause analysis process can help stakeholders (including school staff, students and families, and community members) generate deeper insights about the local needs ...
A root cause analysis process is a systematic investigation of the contributing and foundational (or "root") causes of the problems that organizations or institutions face. 1 In practice, root cause analysis is an approach to problem solving that uses data analysis and discussion to dig deeper than the surface symptoms of a problem to uncover the underlying causes. In recent years ...
Root Cause—the deepest underlying cause, or causes, of positive or negative symptoms within any process that, if dissolved, would result in elimination, or substantial reduction, of the symptom.
There is no single method for conducting a root cause analysis; rather, root cause analysis can be composed of different tools, processes, protocols and perspectives that support a systematic investigation of contributing and foundational causes of challenges; however, there are some common steps in the root cause analysis processes typically used across the public and […]
Root Cause Analysis (RCA) is a problem-solving process designed to unearth the root and fundamental reasons for identified concerns. It requires a systematic investigation of the central causes of the student performance problems that schools and educators may face1. RCA helps educators identify what, how, and why a problem is occurring so it can be addressed more effectively and prevented in ...
10 Examples of Root Cause Analysis. Manufacturing: A computer parts manufacturer identified that their products were failing rapidly due to an underlying design flaw in one of the microchips. So, RCA was conducted, resulting in the development of a new chip designed to eliminate this problem and prevent its recurrence.
The contents of this presentation were developed under a grant from the U.S. Department of Education, #H373Y190001. However, the contents do not necessarily represent the policy of the U.S. Department of Education, and you should not assume endorsement by the federal government.
This step involves identifying the underlying causes behind the priority performance challenges identified during data analysis. Root causes are statements that describe the deepest underlying cause, or causes, of performance challenges and they become the focus of major improvement strategies. In general, the process for determining root ...
This facilitator guide contains protocols designed to engage school leaders and stakeholders in the early steps of a root cause analysis process from identifying a specific, actionable prob-lem and its root causes to prioritizing the root causes for importance and feasibility to address in the school's continuous improvement efforts.
Root cause analysis is an equitable practice because it prevents practitioners and leaders from making assumptions about students and staff, resulting in failure to make change because they were solving problems with the wrong solution.
What is Root Cause Analysis? A structured approach to indentifying the factors that lead to the outcome of a past event in order to to promote the achievement of better future consequences. Root Cause Analysis helps identify what, how and why something happened, thus preventing recurrence. Root causes are underlying, are reasonable identifiable ...
An equity-focused root cause analysis steers attention to what teachers can do to support learning. 3. Recognize and use equitable learning opportunities. A traditional one-size-fits-all approach to learning doesn't acknowledge or respect the unique experiences of different learners.
Root cause analysis is a problem-solving approach that uses the analogy of roots and blooms to model cause-and-effect relationships. Rather than focusing on what's above the surface, root cause analysis troubleshoots solutions to problems by analyzing what is causing them.
Root Cause Analysis (RCA) is defined as a systematic process for identifying the underlying causes or factors that contribute to a problem, incident, or undesirable outcome. Learn more about root cause analysis types, examples, and methods.
Root cause analysis is the process that allows us to move from data to action. The data analysis and identification of challenges and contributing factors tell us what is happening at our schools. Root cause analysis will tell us why it is happening. Once we understand the why, we can then develop targeted interventions to address the challenge.
This root cause analysis process was designed to support Comprehensive Support and Improvement (CSI) schools in identifying evidence-based practices and designing a school improvement plan. This resource profiles what the root cause analysis process looked like from beginning to end in each of these schools, highlighting best practices and key ...
Root cause analysis (RCA) is the process of discovering the root causes of problems in order to identify appropriate solutions. RCA assumes that it is much more effective to systematically prevent and solve for underlying issues rather than just treating ad hoc symptoms and putting out fires. Root cause analysis can be performed with a collection of principles, techniques, and methodologies ...
Root cause analysis is a systematic process whereby the factors that contribute to an incident are identified and learned from.
To answer these questions we need to find the roots of the issues. A Root Cause Analysis can help us do this by inviting us to ask "why" as an entry point for digging deeper rather than a destination for accepting the challenges of education because we care about our students. The Five Whys is a powerful tool to help us do this.
Root Cause Analysis (RCA) is a helpful tool in our problem-solving challenges. Root cause analysis methods involve identifying the root of a problem to arrive at a solution. It helps us dig deeper into the origin of a problem. Additionally, it can help us identify patterns that are inefficient. Organizations deploy several types of root cause ...
Root Cause Analysis or RCA is an analytical tool, technique, or process used to get to the root cause of the problem. Know how root analysis helps us look beyond the superficial cause-and-effect and takes us to the bottom of the failed systems or processes that caused issues in the first place.
Root cause analysis (RCA) is a systematic problem-solving technique used to identify the underlying causes of a particular issue or problem, rather than addressing only its symptoms. It involves a structured approach to investigating and understanding why something happened, with the goal of preventing its recurrence.
This tool describes best practices for conducting a comprehensive Root Cause Analyses and Actions (RCA2) to improve patient safety by reducing medical errors, adverse events, and near misses; the Action Hierarchy tool helps identify which specific actions will have the strongest effect for successful and sustained system improvement.
Root cause analysis with corrective measures : A root cause analysis was performed, and measures were taken to avoid this problem. The RCA team noted that the nurse caring for both patients had worked in the hospital for 5 years and was recently transitioned to the obstetric ward. This had never happened to her before.
Teams that follow observability standards, use monitoring tools, and foster a culture of collaboration can more quickly discover the root cause of system outages and performance issues.
Identifying the root cause of problems is critical in industrial operations. Learn about root cause analysis and its benefits to boost efficiency.