- Heart Disease
- What Is Heart Disease?
- Are You at Risk?
- Types of Heart Disease
- Coronary Artery Disease (CAD)
- Peripheral Artery Disease (PAD)
- Tests & Diagnosis
- Interventions
- Medications
- Living With
- View Full Guide

Heart Disease: Types, Causes, and Symptoms

There are many types of heart disease, and each one has its own symptoms and treatment. For some, lifestyle changes and medicine can make a huge difference in improving your health. For others, you may need surgery to make your ticker work well again.
Find out about some of the common types of heart disease and how to prevent them as well as how they're treated.
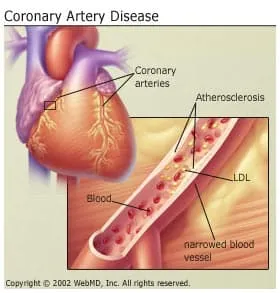
CAD is the most common heart problem. With CAD, you may get blockages in your coronary arteries -- the vessels that supply blood to your heart. That can lead to a decrease in the flow of blood to your heart muscle, keeping it from getting the oxygen it needs. The disease usually starts as a result of atherosclerosis, a condition sometimes called hardening of the arteries.
Coronary heart disease can give you pain in your chest, called angina, or lead to a heart attack .
Some things that may put you at a higher risk of coronary artery disease are:
- Age (For men, the risk of heart disease goes up after age 55; for women, the risk rises sharply after menopause.)
- Being inactive
- Having diabetes or metabolic syndrome
- Family history of coronary heart disease
- High blood pressure
- High levels of LDL "bad" cholesterol or low levels of HDL "good" cholesterol
Heart Arrhythmias
When you have an arrhythmia , your heart has an irregular beating pattern. Serious arrhythmias often develop from other heart problems but may also happen on their own.
- Heart Failure
With heart failure, your heart doesn't pump blood as well as it should to meet your body's needs. It is usually caused by coronary artery disease, but it can also happen because you have thyroid disease, high blood pressure, heart muscle disease (cardiomyopathy), or certain other conditions.
Heart Valve Disease
Your heart has four valves that open and close to direct blood flow between your heart's four chambers, the lungs , and blood vessels. An abnormality could make it hard for a valve to open and close the right way. When that happens, your blood flow could be blocked or blood can leak. Your valve may not open and close right.
The causes of heart valve problems include infections such as rheumatic fever, congenital heart disease, high blood pressure, coronary artery disease, or as a result of a heart attack.
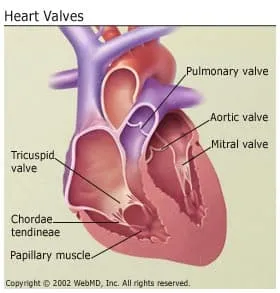
Diseases of the heart valves include:
- Endocarditis. This is an infection that's usually caused by bacteria, which may enter the blood and take root in your heart during illness, after surgery, or after using intravenous drugs. It often happens if you already have valve problems. Antibiotics can usually cure it, but the disease is life-threatening without treatment. If your heart valves are seriously damaged as a result of endocarditis, you may need valve replacement surgery.
- Rheumatic heart disease. This condition develops when your heart muscle and valves are damaged by rheumatic fever, which is linked to strep throat and scarlet fever. Rheumatic heart disease was more common earlier in the 20th century. But doctors are now able to prevent it by using antibiotics to treat the diseases that lead to it. If you do get it, the symptoms usually show up many years after the infection.
Pericardial Disease
Any disease of the pericardium , the sac that surrounds your heart, is called a pericardial disease. One of the more common diseases is pericarditis or inflammation of the pericardium.
It's usually caused by an infection with a virus, inflammatory diseases such as lupus or rheumatoid arthritis, or injury to your pericardium. Pericarditis often follows open heart surgery.
Cardiomyopathy (Heart Muscle Disease)
Cardiomyopathy is a disease of your heart muscle, or myocardium. It gets stretched, thickened, or stiff. Your heart may get too weak to pump well.
There are many possible causes of the disease, including genetic heart conditions, reactions to certain drugs or toxins (such as alcohol), and infections from a virus. Sometimes, chemotherapy causes cardiomyopathy. Many times, doctors can't find the exact cause.
Congenital Heart Disease
Congenital heart disease happens when something goes wrong while the heart is forming in a baby that's still in the womb. The heart abnormality sometimes leads to problems right after birth, but other times there aren't any symptoms until you become an adult.
Septal abnormalities are among the most common congenital heart problems. These are holes in the wall that separates the left and right sides of your heart. You can get a procedure to patch the hole.
Another type of abnormality is called pulmonary stenosis . A narrow valve causes a decrease in the flow of blood to your lungs. A procedure or surgery can open or replace the valve.
In some babies, a small blood vessel known as the ductus arteriosus doesn't close up at birth as it should. When this happens, some blood leaks back into the pulmonary artery, which puts strain on your heart. Doctors can treat this with surgery or a procedure or sometimes with medication.

Top doctors in ,
Find more top doctors on, related links.
- Heart Disease News
- Heart Disease Reference
- Heart Disease Slideshows
- Heart Disease Quizzes
- Heart Disease Videos
- Find a Cardiologist
- Heart Disease Medications
- Book: Take Control of Your Heart Disease Risk
- Abnormal Heart Rhythms
- Atrial Fibrillation
- Cholesterol Management
- High Blood Pressure
- Metabolic Syndrome
- Cholesterol & Your Heart
- More Related Topics

AHA Clinical Update Slides
- Clinical Update Slide Set: 2024 AHA/ACC Guideline on the Management of Lower Extremity Peripheral Artery Disease (PPTX) Published: May 14, 2024
- Clinical Update Slide Set: 2024 Hypertrophic Cardiomyopathy Guideline (PPTX) Published: May 8, 2024
- Clinical Update: 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation Published: November 30, 2023
- Clinical Update Slide Set: Novel Prediction Equations for Absolute Risk Assessment of Total Cardiovascular Disease Incorporating Cardiovascular-Kidney Metabolic Health Slide Set (PPTX) Published: November 10, 2023
- Clinical Update Slide Set: Cardiovascular-Kidney-Metabolic Health: A 2023 Presidential Advisory From the AHA (PPTX) Published: October 9, 2023
- Clinical Update Slide Set: Cardiovascular-Kidney-Metabolic Health (PPTX) Published: October 9, 2023
- Clinical Update Slide Set: 2023 Chronic Coronary Disease Guideline (PPTX) Published: July 20, 2023
- Clinical Update Slide Set: 2023 Aneurysmal Subarachnoid Hemorrhage Guideline (PPTX) Published: May 23, 2023
- Clinical Update Slide Set: 2022 Aortic Disease Guideline (PPTX) Published: November 2, 2022
- Clinical Update Slide Set: 2022 Spontaneous Intracerebral Hemorrhage Guideline (PPTX) Published: May 17, 2022
- Clinical Update Slide Set: 2022 Heart Failure Guideline (PPTX) Published: April 1, 2022
- Clinical Update Slide Set: 2021 Coronary Artery Revascularization Guideline (PPTX) Published: December 9, 2021
- Clinical Update Slide Set: 2021 Chest Pain Guideline (PPTX) Published: October 28, 2021
- 2021 Prevention of Stroke in Patients With Stroke and TIA Guideline (PPTX) Published: May 24, 2021
- Clinical Update Slide Set: 2020 Valvular Heart Disease Guideline (PPTX) Published: December 17, 2020


- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Ischemic Heart Disease
Published by Dustin Chase Modified over 6 years ago
Similar presentations
Presentation on theme: "Ischemic Heart Disease"— Presentation transcript:
Heart - Pathology Ischemic Heart Disease Hypoxemia (diminished transport of oxygen by the blood) less deleterious than ischemia Also called coronary.
Ischemic Heart Disease William J Hunter MD. Types of Heart Disease Acquired Heart Disease Acquired Heart Disease Congenital Heart Disease Congenital Heart.
Prepared by: Dr. Nehad Ahmed. Myocardial infarction or “heart attack” is an irreversible injury to and eventual death of myocardial tissue that results.
Acute Coronary Syndromes. Acute Coronary Syndrome Definition: a constellation of symptoms related to obstruction of coronary arteries with chest pain.
Rick Allen. Acute coronary syndromes include: Unstable angina Acute myocardial infarction Sudden cardiac death Basics of pathophysiology Stable.
Ischemic Heart Disease Group of diseases Most common cause of death in developed countries Terminology: 1.Angina pectoris 2.Myocardial infarction 3.Sudden.
CORONARY CIRCULATION DR. Eman El Eter.
Diseases of the Cardiovascular System Ischemic Heart Disease – Myocardial Infartcion – Sudden Cardiac Death – Heart Failure – Stroke + A Tiny Bit on the.
Ischemic Heart Disease CVS lecture 3 Shaesta Naseem.
Myocardial Ischemia, Injury, and Infarction
Ischemic heart disease
Ischemic Heart Diseases IHD
Dr. Meg-angela Christi M. Amores
Ischemic heart diseases
Cardiovascular practical Block Part I Shaesta Naseem.
1 Dr. Zahoor Ali Shaikh. 2 CORONARY ARTERY DISEASE (CAD) CAD is most common form of heart disease and causes premature death. In UK, 1 in 3 men and.
Ischemic Heart Disease CVS lecture 3
Biochemical Markers of Myocardial Infarction
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Triple Billion
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment case
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
Cardiovascular diseases (CVDs)
- Cardiovascular diseases (CVDs) are the leading cause of death globally.
- An estimated 17.9 million people died from CVDs in 2019, representing 32% of all global deaths. Of these deaths, 85% were due to heart attack and stroke.
- Over three quarters of CVD deaths take place in low- and middle-income countries.
- Out of the 17 million premature deaths (under the age of 70) due to noncommunicable diseases in 2019, 38% were caused by CVDs.
- Most cardiovascular diseases can be prevented by addressing behavioural risk factors such as tobacco use, unhealthy diet and obesity, physical inactivity and harmful use of alcohol.
- It is important to detect cardiovascular disease as early as possible so that management with counselling and medicines can begin.
What are cardiovascular diseases?
Cardiovascular diseases (CVDs) are a group of disorders of the heart and blood vessels. They include:
- coronary heart disease – a disease of the blood vessels supplying the heart muscle;
- cerebrovascular disease – a disease of the blood vessels supplying the brain;
- peripheral arterial disease – a disease of blood vessels supplying the arms and legs;
- rheumatic heart disease – damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria;
- congenital heart disease – birth defects that affect the normal development and functioning of the heart caused by malformations of the heart structure from birth; and
- deep vein thrombosis and pulmonary embolism – blood clots in the leg veins, which can dislodge and move to the heart and lungs.
Heart attacks and strokes are usually acute events and are mainly caused by a blockage that prevents blood from flowing to the heart or brain. The most common reason for this is a build-up of fatty deposits on the inner walls of the blood vessels that supply the heart or brain. Strokes can be caused by bleeding from a blood vessel in the brain or from blood clots.
What are the risk factors for cardiovascular disease?
The most important behavioural risk factors of heart disease and stroke are unhealthy diet, physical inactivity, tobacco use and harmful use of alcohol. The effects of behavioural risk factors may show up in individuals as raised blood pressure, raised blood glucose, raised blood lipids, and overweight and obesity. These “intermediate risks factors” can be measured in primary care facilities and indicate an increased risk of heart attack, stroke, heart failure and other complications.
Cessation of tobacco use, reduction of salt in the diet, eating more fruit and vegetables, regular physical activity and avoiding harmful use of alcohol have been shown to reduce the risk of cardiovascular disease. Health policies that create conducive environments for making healthy choices affordable and available are essential for motivating people to adopt and sustain healthy behaviours.
There are also a number of underlying determinants of CVDs. These are a reflection of the major forces driving social, economic and cultural change – globalization, urbanization and population ageing. Other determinants of CVDs include poverty, stress and hereditary factors.
In addition, drug treatment of hypertension, diabetes and high blood lipids are necessary to reduce cardiovascular risk and prevent heart attacks and strokes among people with these conditions.
What are common symptoms of cardiovascular diseases?
Symptoms of heart attacks and strokes.
Often, there are no symptoms of the underlying disease of the blood vessels. A heart attack or stroke may be the first sign of underlying disease. Symptoms of a heart attack include:
- pain or discomfort in the centre of the chest; and/or
- pain or discomfort in the arms, the left shoulder, elbows, jaw, or back.
In addition the person may experience difficulty in breathing or shortness of breath; nausea or vomiting; light-headedness or faintness; a cold sweat; and turning pale. Women are more likely than men to have shortness of breath, nausea, vomiting, and back or jaw pain.
The most common symptom of a stroke is sudden weakness of the face, arm, or leg, most often on one side of the body. Other symptoms include sudden onset of:
- numbness of the face, arm, or leg, especially on one side of the body;
- confusion, difficulty speaking or understanding speech;
- difficulty seeing with one or both eyes;
- difficulty walking, dizziness and/or loss of balance or coordination;
- severe headache with no known cause; and/or
- fainting or unconsciousness.
People experiencing these symptoms should seek medical care immediately.
What is rheumatic heart disease?
Rheumatic heart disease is caused by damage to the heart valves and heart muscle from the inflammation and scarring caused by rheumatic fever. Rheumatic fever is caused by an abnormal response of the body to infection with streptococcal bacteria, which usually begins as a sore throat or tonsillitis in children.
Rheumatic fever mostly affects children in developing countries, especially where poverty is widespread. Globally, about 2% of deaths from cardiovascular diseases are related to rheumatic heart disease.
Symptoms of rheumatic heart disease
Symptoms of rheumatic heart disease include: shortness of breath, fatigue, irregular heartbeats, chest pain and fainting.
Symptoms of rheumatic fever include: fever, pain and swelling of the joints, nausea, stomach cramps and vomiting.
Why are cardiovascular diseases a development issue in low- and middle-income countries?
At least three-quarters of the world's deaths from CVDs occur in low- and middle-income countries. People living in low- and middle-income countries often do not have the benefit of primary health care programmes for early detection and treatment of people with risk factors for CVDs. People in low- and middle-income countries who suffer from CVDs and other noncommunicable diseases have less access to effective and equitable health care services which respond to their needs. As a result, for many people in these countries detection is often late in the course of the disease and people die at a younger age from CVDs and other noncommunicable diseases, often in their most productive years.
The poorest people in low- and middle-income countries are most affected. At the household level, evidence is emerging that CVDs and other noncommunicable diseases contribute to poverty due to catastrophic health spending and high out-of-pocket expenditure. At the macro-economic level, CVDs place a heavy burden on the economies of low- and middle-income countries.
How can the burden of cardiovascular diseases be reduced?
The key to cardiovascular disease reduction lies in the inclusion of cardiovascular disease management interventions in universal health coverage packages, although in a high number of countries health systems require significant investment and reorientation to effectively manage CVDs.
Evidence from 18 countries has shown that hypertension programmes can be implemented efficiently and cost-effectively at the primary care level which will ultimately result in reduced coronary heart disease and stroke. Patients with cardiovascular disease should have access to appropriate technology and medication. Basic medicines that should be available include:
- beta-blockers;
- angiotensin-converting enzyme inhibitors; and
An acute event such as a heart attack or stroke should be promptly managed.
Sometimes, surgical operations are required to treat CVDs. They include:
- coronary artery bypass;
- balloon angioplasty (where a small balloon-like device is threaded through an artery to open the blockage);
- valve repair and replacement;
- heart transplantation; and
- artificial heart operations.
Medical devices are required to treat some CVDs. Such devices include pacemakers, prosthetic valves, and patches for closing holes in the heart.
WHO response
In 2013, WHO Member States agreed on global mechanisms to reduce the avoidable NCD burden including a "Global action plan for the prevention and control of NCDs 2013-2020". This Plan aims to reduce the number of premature deaths from NCDs by 25% by 2025 through nine voluntary global targets. Two of the targets directly focus on preventing and controlling CVDs.
Target 6: Reduce global prevalence of raised blood pressure by 25% between 2010 and 2025.
Target 8: At least 50% of eligible people should receive drug therapy and counselling (including glycaemic control) to prevent heart attacks and strokes by 2025.
In addition, target 9 states that there should be 80% availability of the affordable basic technologies and essential medicines, including generics, required to treat major NCDs in both public and private facilities.
Achieving these targets will require significant investment in and strengthening of health systems.
WHO is currently working on increasing the normative guidance available for the management of acute coronary syndrome and stroke which will provide guidance in these important areas.
Related links
- Global action plan for the prevention and control of NCDs 2013-2020
- Health topic: cardiovascular diseases
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Cardiovascular disease.
Edgardo Olvera Lopez ; Brian D. Ballard ; Arif Jan .
Affiliations
Last Update: August 22, 2023 .
- Continuing Education Activity
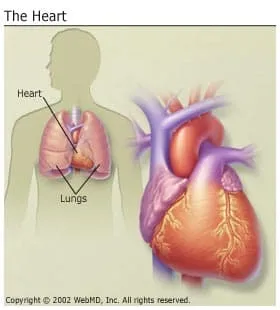
The cardiovascular system consists of the heart and its blood vessels. A wide array of problems can arise within the cardiovascular system, a few of which include endocarditis, rheumatic heart disease, and conduction system abnormalities. Cardiovascular disease, also known as heart disease, refers to the following 4 entities: coronary artery disease (CAD) which is also referred to as coronary heart disease (CHD), cerebrovascular disease, peripheral artery disease (PAD), and aortic atherosclerosis. CAD results from decreased myocardial perfusion that causes angina due to ischemia and can result in myocardial infarction (MI), and/or heart failure. It accounts for one-third to one-half of all cases of cardiovascular disease. Cerebrovascular disease is the entity associated with strokes, also termed cerebrovascular accidents, and transient ischemic attacks (TIAs). Peripheral arterial disease (PAD) is arterial disease predominantly involving the limbs that may result in claudication. Aortic atherosclerosis is the entity associated with thoracic and abdominal aneurysms. This activity reviews the evaluation and treatment of cardiovascular disease and the role of the medical team in evaluating and treating these conditions.
- Review the cause of coronary artery disease.
- Describe the pathophysiology of atherosclerosis.
- Summarize the treatment options for heart disease.
- Outline the evaluation and treatment of cardiovascular disease and the role of the medical team in evaluating and treating this condition.
- Introduction
The cardiovascular system consists of the heart and blood vessels. [1] There is a wide array of problems that may arise within the cardiovascular system, for example, endocarditis, rheumatic heart disease, abnormalities in the conduction system, among others, cardiovascular disease (CVD) or heart disease refer to the following 4 entities that are the focus of this article [2] :
- Coronary artery disease (CAD): Sometimes referred to as Coronary Heart Disease (CHD), results from decreased myocardial perfusion that causes angina, myocardial infarction (MI), and/or heart failure. It accounts for one-third to one-half of the cases of CVD.
- Cerebrovascular disease (CVD): Including stroke and transient ischemic attack (TIA)
- Peripheral artery disease (PAD): Particularly arterial disease involving the limbs that may result in claudication
- Aortic atherosclerosis: Including thoracic and abdominal aneurysms
Although CVD may directly arise from different etiologies such as emboli in a patient with atrial fibrillation resulting in ischemic stroke, rheumatic fever causing valvular heart disease, among others, addressing risks factors associated to the development of atherosclerosis is most important because it is a common denominator in the pathophysiology of CVD.
The industrialization of the economy with a resultant shift from physically demanding to sedentary jobs, along with the current consumerism and technology-driven culture that is related to longer work hours, longer commutes, and less leisure time for recreational activities, may explain the significant and steady increase in the rates of CVD during the last few decades. Specifically, physical inactivity, intake of a high-calorie diet, saturated fats, and sugars are associated with the development of atherosclerosis and other metabolic disturbances like metabolic syndrome, diabetes mellitus, and hypertension that are highly prevalent in people with CVD. [3] [2] [4] [5]
According to the INTERHEART study that included subjects from 52 countries, including high, middle, and low-income countries, 9 modifiable risks factors accounted for 90% of the risk of having a first MI: smoking, dyslipidemia, hypertension, diabetes, abdominal obesity, psychosocial factors, consumption of fruits and vegetables, regular alcohol consumption, and physical inactivity. It is important to mention that in this study 36% of the population-attributable risk of MI was accounted to smoking. [6]
Other large cohort studies like the Framingham Heart Study [7] and the Third National Health and Nutrition Examination Survey (NHANES III) [5] have also found a strong association and predictive value of dyslipidemia, high blood pressure, smoking, and glucose intolerance. Sixty percent to 90% of CHD events occurred in subjects with at least one risk factor.
These findings have been translated into health promotion programs by the American Heart Association with emphasis on seven recommendations to decrease the risk of CVD: avoiding smoking, being physically active, eating healthy, and keeping normal blood pressure, body weight, glucose, and cholesterol levels. [8] [9]
On the other hand, non-modifiable factors as family history, age, and gender have different implications. [4] [7] Family history, particularly premature atherosclerotic disease defined as CVD or death from CVD in a first-degree relative before 55 years (in males) or 65 years (in females) is considered an independent risk factor. [10] There is also suggestive evidence that the presence of CVD risk factors may differently influence gender. [4] [7] For instance, diabetes and smoking more than 20 cigarettes per day had increased CVD risk in women compared to men. [11] Prevalence of CVD increases significantly with each decade of life. [12]
The presence of HIV (human immunodeficiency virus), [13] history of mediastinal or chest wall radiation, [14] microalbuminuria, [15] , increased inflammatory markers [16] [17] have also been associated with an increased rate and incidence of CVD.
Pointing out specific diet factors like meat consumption, fiber, and coffee and their relation to CVD remains controversial due to significant bias and residual confounding encountered in epidemiological studies. [18] [19]
- Epidemiology
Cardiovascular diseases (CVD) remain among the 2 leading causes of death in the United States since 1975 with 633,842 deaths or 1 in every 4 deaths, heart disease occupied the leading cause of death in 2015 followed by 595,930 deaths related to cancer. [2] CVD is also the number 1 cause of death globally with an estimated 17.7 million deaths in 2015, according to the World Health Organization (WHO). The burden of CVD further extends as it is considered the most costly disease even ahead of Alzheimer disease and diabetes with calculated indirect costs of $237 billion dollars per year and a projected increased to $368 billion by 2035. [20]
Although the age-adjusted rate and acute mortality from MI have been declining over time, reflecting the progress in diagnosis and treatment during the last couple of decades, the risk of heart disease remains high with a calculated 50% risk by age 45 in the general population. [7] [21] The incidence significantly increases with age with some variations between genders as the incidence is higher in men at younger ages. [2] The difference in incidence narrows progressively in the post-menopausal state. [2]
- Pathophysiology
Atherosclerosis is the pathogenic process in the arteries and the aorta that can potentially cause disease as a consequence of decreased or absent blood flow from stenosis of the blood vessels. [22]
It involves multiple factors dyslipidemia, immunologic phenomena, inflammation, and endothelial dysfunction. These factors are believed to trigger the formation of fatty streak, which is the hallmark in the development of the atherosclerotic plaque [23] ; a progressive process that may occur as early as in the childhood. [24] This process comprises intimal thickening with subsequent accumulation of lipid-laden macrophages (foam cells) and extracellular matrix, followed by aggregation and proliferation of smooth muscle cells constituting the formation of the atheroma plaque. [25] As this lesions continue to expand, apoptosis of the deep layers can occur, precipitating further macrophage recruitment that can become calcified and transition to atherosclerotic plaques. [26]
Other mechanisms like arterial remodeling and intra-plaque hemorrhage play an important role in the delay and accelerated the progression of atherosclerotic CVD but are beyond the purpose of this article. [27]
- History and Physical
The clinical presentation of cardiovascular diseases can range from asymptomatic (e.g., silent ischemia, angiographic evidence of coronary artery disease without symptoms, among others) to classic presentations as when patients present with typical anginal chest pain consistent of myocardial infarction and/or those suffering from acute CVA presenting with focal neurological deficits of sudden onset. [28] [29] [28]
Historically, coronary artery disease typically presents with angina that is a pain of substernal location, described as a crushing or pressure in nature, that may radiate to the medial aspect of the left upper extremity, to the neck or the jaw and that can be associated with nausea, vomiting, palpitations, diaphoresis, syncope or even sudden death. [30] Physicians and other health care providers should be aware of possible variations in symptom presentation for these patients and maintain a high index of suspicion despite an atypical presentation, for example, dizziness and nausea as the only presenting symptoms in patients having an acute MI [31] ), particularly in people with a known history of CAD/MI and for those with the presence of CVD risk factors. [32] [33] [34] [33] [32] Additional chest pain features suggestive of ischemic etiology are the exacerbation with exercise and or activity and resolution with rest or nitroglycerin. [35]
Neurologic deficits are the hallmark of cerebrovascular disease including TIA and stroke where the key differentiating factor is the resolution of symptoms within 24 hours for patients with TIA. [36] Although the specific symptoms depend on the affected area of the brain, the sudden onset of extremity weakness, dysarthria, and facial droop are among the most commonly reported symptoms that raise concern for a diagnosis of a stroke. [37] [38] Ataxia, nystagmus and other subtle symptoms as dizziness, headache, syncope, nausea or vomiting are among the most reported symptoms with people with posterior circulation strokes challenging to correlate and that require highly suspicion in patients with risks factors. [39]
Patients with PAD may present with claudication of the limbs, described as a cramp-like muscle pain precipitated by increased blood flow demand during exercise that typically subsides with rest. [40] Severe PAD might present with color changes of the skin and changes in temperature. [41]
Most patients with thoracic aortic aneurysm will be asymptomatic, but symptoms can develop as it progresses from subtle symptoms from compression to surrounding tissues causing cough, shortness of breath or dysphonia, to the acute presentation of sudden crushing chest or back pain due to acute rupture. [42] The same is true for abdominal aortic aneurysms (AAA) that cause no symptoms in early stages to the acute presentation of sudden onset of abdominal pain or syncope from acute rupture. [43]
A thorough physical examination is paramount for the diagnosis of CVD. Starting with a general inspection to look for signs of distress as in patients with angina or with decompensated heart failure, or chronic skin changes from PAD. Carotid examination with the patient on supine position and the back at 30 degrees for the palpation and auscultation of carotid pulses, bruits and to evaluate for jugular venous pulsations on the neck is essential. Precordial examination starting with inspection, followed by palpation looking for chest wall tenderness, thrills, and identification of the point of maximal impulse should then be performed before auscultating the precordium. Heart sounds auscultation starts in the aortic area with the identification of the S1 and S2 sounds followed by characterization of murmurs if present. Paying attention to changes with inspirations and maneuvers to correctly characterize heart murmurs is encouraged. Palpating peripheral pulses with bilateral examination and comparison when applicable is an integral part of the CVD examination. [44]
Thorough clinical history and physical exam directed but not limited to the cardiovascular system are the hallmarks for the diagnosis of CVD. Specifically, a history compatible with obesity, angina, decreased exercise tolerance, orthopnea, paroxysmal nocturnal dyspnea, syncope or presyncope, and claudication should prompt the clinician to obtain a more detailed history and physical exam and, if pertinent, obtain ancillary diagnostic test according to the clinical scenario (e.g., electrocardiogram and cardiac enzymes for patients presenting with chest pain).
Besides a diagnosis prompted by clinical suspicion, most of the efforts should be oriented for primary prevention by targeting people with the presence of risk factors and treat modifiable risk factors by all available means. All patient starting at age 20 should be engaged in the discussion of CVD risk factors and lipid measurement. [9] Several calculators that use LDL-cholesterol and HDL-cholesterol levels and the presence of other risk factors calculate a 10-year or 30-year CVD score to determine if additional therapies like the use of statins and aspirin are indicated for primary prevention, generally indicated if such risk is more than ten percent. [10] Like other risk assessment tools, the use of this calculators have some limitations, and it is recommended to exert precaution when assessing patients with diabetes and familial hypercholesterolemia as their risk can be underestimated. Another limitation to their use is that people older than 79 were usually excluded from the cohorts where these calculators were formulated, and individualized approach for these populations is recommended by discussing risk and benefits of adjunctive therapies and particular consideration of life expectancy. Some experts recommend a reassessment of CVD risk every 4 to 6 years. [9]
Preventative measures like following healthy food habits, avoiding overweight and following an active lifestyle are pertinent in all patients, particularly for people with non-modifiable risk factors such as family history of premature CHD or post-menopause. [9] [8]
The use of inflammatory markers and other risk assessment methods as coronary artery calcification score (CAC) are under research and have limited applications that their use should not replace the identification of people with known risk factors, nonetheless these resources remain as promising tools in the future of primary prevention by detecting people with subclinical atherosclerosis at risk for CVD. [45]
- Treatment / Management
Management of CVD is very extensive depending on the clinical situation (catheter-directed thrombolysis for acute ischemic stroke, angioplasty for peripheral vascular disease, coronary stenting for CHD); however, patients with known CVD should be strongly educated on the need for secondary prevention by risk factor and lifestyle modification. [9] [46]
- Differential Diagnosis
- Acute pericarditis
- Angina pectoris
- Artherosclerosis
- Coronary artery vasospasm
- Dilated cardiomyopathy
- Giant cell arteritis
- Hypertension
- Hypertensive heart disease
- Kawasaki disease
- Myocarditis
The prognosis and burden of CVD have been discussed in other sections.
- Complications
The most feared complication from CVD is death and, as explained above, despite multiple discoveries in the last decades CVD remains in the top leading causes of death all over the world owing to the alarming prevalence of CVD in the population. [2] Other complications as the need for longer hospitalizations, physical disability and increased costs of care are significant and are the focus for health-care policymakers as it is believed they will continue to increase in the coming decades. [20]
For people with heart failure with reduced ejection fraction (HFreEF) of less than 35%, as the risk of life-threatening arrhythmias is exceedingly high in these patients, current guidelines recommend the implantation of an implantable-cardioverter defibrillator (ICD) for those with symptoms equivalent to a New York Heart Association (NYHA) Class II-IV despite maximal tolerated medical therapy. [47]
Strokes can leave people with severe disabling sequelae like dysarthria or aphasia, dysphagia, focal or generalized muscle weakness or paresis that can be temporal or cause permanent physical disability that may lead to a complete bedbound state due to hemiplegia with added complications secondary to immobility as is the higher risk of developing urinary tract infections and/or risk for thromboembolic events. [48] [49]
There is an increased risk of all-cause death for people with PAD compared to those without evidence of peripheral disease. [50] Chronic wounds, physical limitation, and limb ischemia are among other complications from PAD. [51]
- Consultations
An interprofessional approach that involves primary care doctors, nurses, dietitians, cardiologists, neurologists, and other specialists is likely to improve outcomes. This has been shown to be beneficial in patients with heart failure, [52] coronary disease, [53] and current investigations to assess the impact on other forms of CVD are under planning and promise encouraging results.
- Deterrence and Patient Education
Efforts should be directed toward primary prevention by leading a healthy lifestyle, and an appropriate diet starting as early as possible with the goal of delay or avoid the initiation of atherosclerosis as it relates to the future risk of CVD. The AHA developed the concept of "ideal cardiovascular health" defined by the presence of [8] :
- Ideal health behaviors: Nonsmoking, body mass index less than 25 kg/m2, physical activity at goal levels, and the pursuit of a diet consistent with current guideline recommendations
- Ideal health factors: Untreated total cholesterol less than 200 mg/dL, untreated blood pressure less than 120/80 mm Hg, and fasting blood glucose less than 100 mg/dL) with the goal to improve the health of all Americans with an expected decrease in deaths from CVD by 20%
Specific attention should be made to people at higher risk for CVD as are people with diabetes, hypertension, hyperlipidemia, smokers, and obese patients. Risk factors modification by controlling their medical conditions, avoiding smoking, taking appropriate measures to lose weight and maintaining an active lifestyle is of extreme importance. [8] [9] [10] The recommendations on the use of statins and low-dose aspirin for primary and secondary prevention has been discussed in other sections.
- Pearls and Other Issues
Cardiovascular disease generally refers to 4 general entities: CAD, CVD, PVD, and aortic atherosclerosis.
CVD is the main cause of death globally.
Measures aimed to prevent the progression of atherosclerosis are the hallmark for primary prevention of CVD.
Risk factor and lifestyle modification are paramount in the prevention of CVD.
- Enhancing Healthcare Team Outcomes
An interprofessional and patient-oriented approach can help to improve outcomes for people with cardiovascular disease as shown in patients with heart failure (HF) who had better outcomes when the interprofessional involvement of nurses, dietitians, pharmacists, and other health professionals was used (Class 1A). [52]
Similarly, positive results were obtained in people in an intervention group who were followed by an interprofessional team comprised of pharmacists, nurses and a team of different physicians. This group had a reduction in all-cause mortality associated with CAD by 76% compared to the control group. [53] Healthcare workers should educate the public on lifestyle changes and reduce the modifiable risk factors for heart disease to a minimum.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Atherosclerosis as a result of coronary heart disease. Contributed by National Heart, Lung and Blood Institute (NIH)
Coronary Artery Disease Pathophysiology. Coronary artery disease is usually caused by an atherosclerotic plaque that blocks the lumen of a coronary artery, typically the left anterior descending artery. Contributed by S Bhimji, MD
Disclosure: Edgardo Olvera Lopez declares no relevant financial relationships with ineligible companies.
Disclosure: Brian Ballard declares no relevant financial relationships with ineligible companies.
Disclosure: Arif Jan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Olvera Lopez E, Ballard BD, Jan A. Cardiovascular Disease. [Updated 2023 Aug 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review De-risking primary prevention: role of imaging. [Ther Adv Cardiovasc Dis. 2021] Review De-risking primary prevention: role of imaging. Shafter AM, Shaikh K, Johanis A, Budoff MJ. Ther Adv Cardiovasc Dis. 2021 Jan-Dec; 15:17539447211051248.
- Shared and non-shared familial susceptibility of coronary heart disease, ischemic stroke, peripheral artery disease and aortic disease. [Int J Cardiol. 2013] Shared and non-shared familial susceptibility of coronary heart disease, ischemic stroke, peripheral artery disease and aortic disease. Calling S, Ji J, Sundquist J, Sundquist K, Zöller B. Int J Cardiol. 2013 Oct 3; 168(3):2844-50. Epub 2013 Apr 30.
- Stenting for peripheral artery disease of the lower extremities: an evidence-based analysis. [Ont Health Technol Assess Ser....] Stenting for peripheral artery disease of the lower extremities: an evidence-based analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2010; 10(18):1-88. Epub 2010 Sep 1.
- Impact of cardiovascular disease on health care economic burden and resource utilization: a retrospective cohort study in adults in the United States with type 2 diabetes with or without stroke, myocardial infarction, and peripheral arterial disease. [Curr Med Res Opin. 2022] Impact of cardiovascular disease on health care economic burden and resource utilization: a retrospective cohort study in adults in the United States with type 2 diabetes with or without stroke, myocardial infarction, and peripheral arterial disease. King A, Rajpura J, Liang Y, Paprocki Y, Uzoigwe C. Curr Med Res Opin. 2022 Nov; 38(11):1831-1840. Epub 2022 Sep 29.
- Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? [Am J Ther. 2004] Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? Bacaner M, Brietenbucher J, LaBree J. Am J Ther. 2004 Sep-Oct; 11(5):366-411.
Recent Activity
- Cardiovascular Disease - StatPearls Cardiovascular Disease - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Heart Disease
The following presentations provide information on heart disease.
The files will download in a Powerpoint presentation format when you click on the title.
- Alcohol and the Heart
- Cholesterol and the Heart
- Exercise and the Heart
- Heart Healthy Foods
- Stress and the Heart
Centers & Institutes

Metabolic Basis of Disease Center
Institute for Dementia Research & Prevention
Louisiana Clinical & Translational Science Center
Nutrition Obesity Research Center
Metamor Institute
Center for Military Performance & Resilience
Childhood Obesity and Diabetes Research
Human Research Protections Program
Research Kitchen + Recipes
Business Development
LAUNCHED Program
Pennington Biomedical Research Foundation
Our Partners
Obesity Society
American Diabetes Association
Sign Up For Updates
6400 Perkins Rd. Baton Rouge, LA 70808 ph: (225) 763-2500 fax: (225) 763-3022
© Copyright Pennington Biomedical Research Center
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Heart Disease
- Risk Factors
- Heart Disease Facts
- Healthy People 2030
- Heart Disease Communications Toolkit
- Publication
- Community-Clinical Linkages Health Equity Guide
- Emergency Medical Services (EMS) Home Rule State Law Fact Sheet
- American Heart Month Toolkits
- Healthy Eating Communications Kit
Related Topics:
- About Stroke
- About High Blood Pressure
- About Cholesterol
Preventing Heart Disease
You can choose healthy habits to help prevent heart disease.
- Take charge of your medical conditions to lower your risk for heart disease.

By living a healthy lifestyle, you can help keep your blood pressure, cholesterol, and blood sugar levels normal and lower your risk for heart disease and heart attack.
Choose healthy habits
Choose healthy food and drinks.
Choose healthy meals and snacks to help prevent heart disease and its complications. Be sure to eat plenty of fresh fruits and vegetables and fewer processed foods.
- Eating lots of foods high in saturated fat and trans fat may contribute to heart disease.
- Eating foods high in fiber and low in saturated fats, trans fat, and cholesterol can help prevent high cholesterol.
- Limiting salt (sodium) in your diet can also lower your blood pressure.
- Limiting sugar in your diet can lower your blood sugar level to prevent or help control diabetes.
- Do not drink too much alcohol, which can raise your blood pressure.
Keep a healthy weight
People with overweight or obesity have a higher risk for heart disease. Carrying extra weight can put extra stress on the heart and blood vessels.
To find out if your weight is in a healthy range, you can calculate your Body Mass Index (BMI).
Get regular physical activity
Physical activity can help you maintain a healthy weight and lower your blood pressure, blood cholesterol, and blood sugar levels. For adults, the Surgeon General recommends 2 hours and 30 minutes of moderate-intensity exercise, like brisk walking or bicycling, every week. Children and adolescents should get 1 hour of physical activity every day.
Don't smoke
Cigarette smoking greatly increases your risk for heart disease. If you don't smoke, don't start. If you do smoke, quitting will lower your risk for heart disease. Your doctor can suggest ways to help you quit.
For more information about tobacco use and quitting, see CDC's Smoking & Tobacco Use website .
Take charge of your medical conditions
If you have high cholesterol, high blood pressure, or diabetes, you can take steps to lower your risk for heart disease.
Check your cholesterol
Your health care team should test your blood levels of cholesterol at least once every 4 to 6 years. If you have already been diagnosed with high cholesterol or have a family history of the condition, you may need to have your cholesterol checked more often. Talk with your health care team about this simple blood test. If you have high cholesterol, medicines and lifestyle changes can help reduce your risk for heart disease.
Control your blood pressure
High blood pressure usually has no symptoms, so have it checked on a regular basis. Your health care team should measure your blood pressure at least once every 2 years if you have never had high blood pressure or other risk factors for heart disease.
If you have been diagnosed with high blood pressure, also called hypertension, your health care team will measure your blood pressure more often to make sure you have the condition under control. Talk with your health care team about how often you should check your blood pressure. You can check it at a doctor's office, at a pharmacy, or at home.
If you have high blood pressure, your health care team might recommend some changes in your lifestyle, such as lowering the sodium in your diet. Your doctor may also prescribe medicine to help lower your blood pressure.
Manage your diabetes
If you have diabetes, monitor your blood sugar levels carefully. Talk with your health care team about treatment options. Your doctor may recommend certain lifestyle changes to help keep your blood sugar under control. These actions will help reduce your risk for heart disease.
Take your medicines as directed
If you take medicine to treat high blood cholesterol, high blood pressure, or diabetes, follow your doctor’s instructions carefully. Always ask questions if you don’t understand something. Never stop taking your medicine without first talking to your doctor, nurse, or pharmacist.
Work with your health care team
You and your health care team can work together to prevent or treat the medical conditions that lead to heart disease. Discuss your treatment plan regularly, and bring a list of questions to your appointments. Talk with your health care team about how heart disease and mental health disorders are related .
If you've already had a heart attack , your health care team will work with you to prevent another one. Your treatment plan may include medicines or surgery and lifestyle changes to reduce your risk. Be sure to take your medicines as directed and follow your doctor's instructions.
- Million Hearts ® ABCS of Heart Health
- USDA Center for Nutrition Policy and Promotion – Dietary Guidelines
Heart Disease
Heart disease is the leading cause of death in the United States.
For Everyone
Public health.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

26 templates
6 templates

first day of school
68 templates
72 templates

indigenous canada
8 templates
48 templates
Heart Presentation templates
We wholeheartedly want to invite you to pour all your heart into editing these amazing presentations about hearts this is the strongest muscle in your body and it never rests, it’s always working for you. speak about it with these designs where this organ is the protagonist and edit them, your public will skip a beat when they see your presentation.

It seems that you like this template!
Coronary heart disease.
Coronary heart disease (CHD) is a very common complication that blocks the arteries of the heart. It is caused by the accumulation of fats in your bloodstream and can cause chest pains, shortness of breath, feeling weak or sick… You might also have heard about atherosclerosis. It’s a synonym for...

Premium template
Unlock this template and gain unlimited access
Anatomy of a Heart
The heart is arguably the most important organ in the human body, and it's amazing to think about all the complex functions it performs. It supplies precious oxygen and nutrients with every beat. It truly is an incredible machine that deserves all the care and attention we can give it....

Cardiovascular Diseases: Arrhythmia Infographics
Download the Cardiovascular Diseases: Arrhythmia Infographics template for PowerPoint or Google Slides and discover the power of infographics. An infographic resource gives you the ability to showcase your content in a more visual way, which will make it easier for your audience to understand your topic. Slidesgo infographics like this...

Lovely Hearts Theme
Download the Lovely Hearts Theme presentation for PowerPoint or Google Slides and start impressing your audience with a creative and original design. Slidesgo templates like this one here offer the possibility to convey a concept, idea or topic in a clear, concise and visual way, by using different graphic resources....

Cardiovsacular Diseases: Heart Failure
Download the Cardiovsacular Diseases: Heart Failure presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking...

Science Subject for Middle School: Heart Anatomy
Download the Science Subject for Middle School: Heart Anatomy presentation for PowerPoint or Google Slides. If you’re looking for a way to motivate and engage students who are undergoing significant physical, social, and emotional development, then you can’t go wrong with an educational template designed for Middle School by Slidesgo!...

Lovely Hearts Consulting Toolkit
Imagine that a client is looking for the services of a consultant so that they can come up with suggestions to improve the company's performance. Wouldn't it be so surprising if the presentation they use is super lovely? The business world is so competitive, sometimes you just need a little...

World Heart Day
Mark on your calendar September 29th because it is World Heart Day. This day is very important because cardiovascular diseases affect a large number of people around the world. A malfunction of our heart can be caused by different factors, such as diabetes or smoking. Giving visibility to this issue...

Heart Failure Clinical Case
Clinical cases help medical investigators and students to better understand diseases, their causes and treatments. For instance, keeping track of a patient with a heart disease can help future patients find a cure faster and more efficiently. But you need a presentation with lots of medical resources in order to...
Cardiovascular Disease
It’s time to talk about cardiovascular diseases. Provide some data about them using this creative template full of illustrations of hearts, body diagrams, tables. We have also added useful sections to share data about the diagnosis, recommendations, pathology, treatment and processes.

Coronary Heart Disease Infographics
Download the Coronary Heart Disease Infographics template for PowerPoint or Google Slides and discover the power of infographics. An infographic resource gives you the ability to showcase your content in a more visual way, which will make it easier for your audience to understand your topic. Slidesgo infographics like this...

Hypertrophic Cardiomyopathy Disease
Hypertrophic cardiomyopathy. Sounds like a complicated concept, doesn't it? If you talk about it with your expert medical colleagues, they won't have any doubts, but maybe things get difficult when you want to make a presentation to a non-expert audience. That's okay! Slidesgo is here to help you. This template...
Cardiovascular Diseases: Arrhythmia
Boom, boom. You hear it? It’s you heart sending blood to every inch of your body, it has always done it and it will for the rest of your life. But sometimes, boom might be a bit too fast, or too slow. Arrythmia happens when the pounding rhythm of your...

Cute Kawaii Style Portfolio
Download the Cute Kawaii Style Portfolio presentation for PowerPoint or Google Slides. When a potential client or employer flips through the pages of your portfolio, they're not just looking at your work; they're trying to get a sense of who you are as a person. That's why it's crucial to...

Ventricular Septal Defects Clinical Case Report
Ventricular Septal Defects (VSDs) are a common type of congenital heart defect that can have a range of symptoms and severity levels. They occur when a hole opens up in the wall that separates the two lower chambers of the heart, causing oxygen-rich blood to mix with oxygen-poor blood. In...

Congenital Heart Defect Awareness Week
There's an important time of year; the period between February 7 to 14, marking Congenital Heart Defect Awareness Week! An appropriate time to highlight this often silent illness and recognize all those who have been afflicted by it, and to celebrate the progress that has been made in terms of...

Treatment of Heart Diseases Breakthrough
Download the Treatment of Heart Diseases Breakthrough presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should there...
Cardiac Failure
Download the "Cardiac Failure" presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical attention....
- Page 1 of 10

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Slide Set | 2020 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease
Download PowerPoint File
See Also: Guideline Hub | Valvular Heart Disease
Date: December 17, 2020
Keywords: Anticoagulants, Fibrinolytic Agents, Platelet Aggregation Inhibitors, Aortic Valve Insufficiency, Aortic Valve Stenosis, Aortic Valve, Aortic Diseases, Perioperative Period, Cardiac Catheterization, Cardiac Imaging Techniques, Magnetic Resonance Imaging, Cardiovascular Surgical Procedures, Diagnostic Techniques, Cardiovascular, Drug Therapy, Echocardiography, Endocarditis, Exercise Test, Diagnostic Imaging, Angiography, Hemodynamics, Mitral Valve Stenosis, Mitral Valve Insufficiency, Heart Murmurs, Mitral Valve, Pregnancy, Heart Valve Prosthesis, Decision Making, Heart Valve Diseases, Heart Defects, Congenital, Patient Care Team, Thromboembolism, Thrombosis, Transcatheter Aortic Valve Replacement, Heart Valve Prosthesis Implantation, Catheters, Echocardiography, Transesophageal, Tricuspid Valve
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Contact Member Care
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Watch CBS News
61% of U.S. adults will have some type of cardiovascular disease by 2050, report finds
By Sara Moniuszko
Edited By Allison Elyse Gualtieri
June 4, 2024 / 5:00 AM EDT / CBS News
Cardiovascular disease is the leading cause of death and disability in the United States — and new projections find it may become even more common in the next 30 years.
In a report released Tuesday, the American Heart Association says more than 6 in 10 U.S. adults (61%) will have some type of cardiovascular disease, or CVD, by 2050. This is particularly driven by a projected 184 million people with hypertension, or high blood pressure , which is expected to increase from 51.2% in 2020 to 61% in 2025.
"Clinically, cardiovascular disease is identified as a number of specific conditions, including coronary heart disease (including heart attack), arrhythmias (including atrial fibrillation), valvular disease, congenital heart disease, heart failure, stroke and hypertension," the association defines in its report. "However, high blood pressure is also known as a major risk factor contributing to both heart disease and stroke."
Where are other increases expected?
Total CVD diagnoses, which includes numbers for stroke but not high blood pressure, will increase from 11.3% to 15% or from 28 million to 45 million adults, during the same time.
Stroke specifically will see the largest increase, according to the report, jumping from 3.9% to 6.4%, with the "total prevalence number nearly doubling from 10 million to almost 20 million adults."
Increases were also projected for coronary heart disease (from 7.8% to 9.2%) and heart failure (from 2.7% to 3.8%).
And while there is a projected decline of high cholesterol diagnoses, other risk factors like obesity and diabetes will also increase, from 43.1% to 60.6% and 16.3% to 26.8%, respectively.
Prevalence also varies by racial and ethnic groups, the report found. For example, the increase in total projected numbers of people with CVD and poor health behaviors rose most among Hispanic adults and Asian populations, while Black adults are projected to have the highest prevalence of hypertension, diabetes and obesity.
These disparities can be attributed to "individual, structural and systemic racism, as well as socioeconomic factors and access to care," the report notes.
- These 6 heart attack symptoms in women are key signs to look out for, doctor shares
- How improving sleep can mean better cardiac health
- American Heart Association
- Heart Disease
Sara Moniuszko is a health and lifestyle reporter at CBSNews.com. Previously, she wrote for USA Today, where she was selected to help launch the newspaper's wellness vertical. She now covers breaking and trending news for CBS News' HealthWatch.
More from CBS News

New COVID variant KP.3 climbs to 25%, now largest in CDC estimates
FDA approves first RSV vaccine for adults in their 50s

After an MS diagnosis, this man started running marathons

Proposed heat rules for California would keep workers, schoolchildren cool
COVID-19: Who's at higher risk of serious symptoms?
Advanced age and some health conditions can raise the risk of serious COVID-19 (coronavirus disease 2019) illness.
Many people with COVID-19, also called coronavirus disease 2019, recover at home. But for some, COVID-19 can be a serious illness. Some people may need care in the hospital, treatment in the intensive care unit and the need for breathing help. In some people, severe COVID-19 illness can lead to death.
What raises the risk of severe or critical COVID-19 illness?
The risk for serious COVID-19 illness depends on your health status, age and activities. Your risk also depends on other factors. This includes where you live, work or learn, how easy it is for you to get medical care, and your economic stability.
If you have more than one risk factor, your risk goes up with each one.
Age raises the risk of serious COVID-19
People age 65 and older and babies younger than 6 months have a higher than average risk of serious COVID-19 illness. Those age groups have the highest risk of needing hospital care for COVID-19.
Babies younger than 6 months aren't eligible for the COVID-19 vaccine, which adds to their risk. For older people, the challenge is that the immune system is less able to clear out germs as people age. Also, as people age, medical conditions that raise the risk of severe COVID-19 are more likely. In the U.S. as of March 2024, about 76% of all deaths from COVID-19 have been among people age 65 and older.
Aging plus disease raises the risk of serious COVID-19
Severe COVID-19 disease is more likely for people who have other health issues.
Some common diseases linked to aging are:
- Heart disease. Examples are heart failure or coronary artery disease.
- Diabetes mellitus. The risk is higher for both type 1 and type 2.
- Chronic lung diseases. This includes airway disease and conditions that damage lung tissue.
- Obesity. The risk goes up as body mass index (BMI) increases, with the highest risk for a BMI of 40 or greater.
- Chronic kidney disease. Especially if you are on dialysis.
These diseases become more common as people age. But they can affect people of any age. The risk of serious COVID-19 illness is linked to having one or more underlying medical condition.
Asthma, COPD, other lung diseases raise risk of severe COVID-19
Your risk of having more severe COVID-19 illness is higher if you have lung disease. Having moderate to severe asthma raises some risks of serious COVID-19 illness. It raises the risk of needing care in the hospital, including intensive care, and needing mechanical help breathing.
The risk of serious COVID-19 illness also is higher for people who have conditions that damage lung tissue over time. Examples are tuberculosis, cystic fibrosis, interstitial lung disease, bronchiectasis or COPD, which stands for chronic obstructive pulmonary disease. These diseases raise the risk of needing care in the hospital for COVID-19. Depending on the condition, the risk of needing intensive care and the risk of death from COVID-19 also may go up.
Other lung conditions, such as a history of pulmonary hypertension or pulmonary embolism affect a person's risk of serious illness after COVID-19. The risk of death may be higher after these conditions.
Cancer raises the risk of severe COVID-19
In general, people with cancer have a greater risk of getting serious COVID-19. People who have or had blood cancer may have a higher risk of being sick for longer, or getting sicker, with COVID-19 than people with solid tumors.
Having cancer raises the risk of needing care in the hospital, intensive care and the use of breathing support. Having blood cancer and getting COVID-19 raises the risk of death from the illness.
Treatment for blood cancer may raise the risk of severe COVID-19 but the research is still unclear. Cancer treatment may also affect your COVID-19 vaccine. Talk to your healthcare professional about additional shots and getting vaccinated after treatments that affect some immune cells.
Other conditions that raise the risk of severe COVID-19
If an organ or body system is already weakened by disease, infection with the COVID-19 virus can cause further damage. In other cases, medicine for the original condition can lower the immune system's response to the virus that causes COVID-19.
Many different diseases can raise the risk of severe COVID-19 illness.
- Brain and nervous system diseases, such as strokes.
- Chronic liver disease, specifically cirrhosis, nonalcoholic fatty liver disease, alcoholic liver disease and autoimmune hepatitis.
- HIV not well managed with medicine.
- Heart disease, including congenital heart disease and cardiomyopathies.
- Mood disorders or schizophrenia.
- Having received an organ or stem cell transplant.
- Sickle cell anemia and thalassemia blood disorders.
Other risk factors for severe COVID-19 are:
- Not getting enough physical activity.
- Pregnancy or having recently given birth.
- Use of medicines that lower the immune system's ability to respond to germs.
Also, as a general group, disability is linked to an increased risk of severe COVID-19. The risks are different depending on the disability.
- Down syndrome is linked to a higher risk of needing care in the hospital. The risk of death from severe COVID-19 also is higher than typical for people with Down syndrome.
- Attention deficit/hyperactivity disorder is linked to an increased risk of needing care in the hospital from severe COVID-19.
- Cerebral palsy is linked to an increased risk of needing care in the hospital from severe COVID-19.
These are not the only conditions that increase the risk of severe COVID-19. Talk to your healthcare professional if you have questions about your health and risk for getting a serious COVID-19 illness.
A COVID-19 vaccine can lower your risk of serious illness
The COVID-19 vaccine can lower the risk of death or serious illness caused by COVID-19. Your healthcare team may suggest added doses of COVID-19 vaccine if you have a moderately or seriously weakened immune system.
How else can you lower the risk of severe COVID-19?
Everyone can lower the risk of serious COVID-19 illness by working to prevent infection with the virus that causes COVID-19.
- Avoid close contact with anyone who is sick or has symptoms, if possible.
- Use fans, open windows or doors, and use filters to move the air and keep any germs from lingering.
- Wash your hands well and often with soap and water for at least 20 seconds. Or use an alcohol-based hand sanitizer with at least 60% alcohol.
- Cough or sneeze into a tissue or your elbow. Then wash your hands.
- Clean and disinfect high-touch surfaces. For example, clean doorknobs, light switches, electronics and counters regularly.
- Spread out in crowded public areas, especially in places with poor airflow. This is important if you have a higher risk of serious illness.
- The U.S. Centers for Disease Control and Prevention recommends that people wear a mask in indoor public spaces if COVID-19 is spreading. This means if you're in an area with a high number of people with COVID-19 in the hospital. They suggest wearing the most protective mask possible that you'll wear regularly, that fits well and is comfortable.
These basic actions are even more important for people who have weakened immune systems, and their caregivers.
The FDA also has authorized the monoclonal antibody pemivibart (Pemgarda) to prevent COVID-19 in some people with weakened immune systems.
People can take other actions based on their risk factors.
- If you're at a higher risk of serious illness, talk to your healthcare professional about how best to protect yourself. Know what to do if you get sick so you can quickly start treatment.
- Lower your risk of COVID-19 complications by making sure that any health issues are well managed. This includes staying on track with managing medical conditions, going to all healthcare appointments and planning ahead to avoid running out of medicine. Keep taking medicines as suggested by your healthcare professional.
- Stay up to date on vaccines. This includes vaccines for flu, pneumonia and RSV. These vaccines won't prevent COVID-19. But becoming ill with a respiratory illness may worsen your outcome if you also catch COVID-19.
You may consider making a care plan. In the care plan, write your medical conditions, the medicine you take, and any special food or diet needs you have. The care plan also includes who you see for care and your emergency contacts.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Goldman L, et al., eds. COVID-19: Epidemiology, clinical manifestations, diagnosis, community prevention, and prognosis. In: Goldman-Cecil Medicine. 27th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed April 5, 2024.
- Regan JJ, et al. Use of Updated COVID-19 Vaccines 2023-2024 Formula for Persons Aged ≥6 Months: Recommendations of the Advisory Committee on Immunization Practices—United States, September 2023. MMWR. Morbidity and Mortality Weekly Report 2023; doi:10.15585/mmwr.mm7242e1.
- Underlying medical conditions associated with higher risk for severe COVID-19: Information for healthcare providers. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html. Accessed April 2, 2024.
- Stay up to date with COVID-19 vaccines. Centers for Disease Control and Prevention. www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed April 2, 2024.
- COVID data tracker. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#demographics. Accessed April 2, 2024.
- Najafabadi BT, et al. Obesity as an independent risk factor for COVID‐19 severity and mortality. Cochrane Database of Systematic Reviews. 2023; doi:10.1002/14651858.CD015201.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed April 2, 2024.
- AskMayoExpert. COVID-19: Outpatient management (adult). Mayo Clinic; 2023.
- Emergency use authorizations for drugs and non-vaccine biological products. U.S. Food and Drug Association. https://www.fda.gov/drugs/emergency-preparedness-drugs/emergency-use-authorizations-drugs-and-non-vaccine-biological-products. Accessed April 2, 2024.
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed April 2, 2024.
- COVID-19: What people with cancer should know. National Cancer Institute. https://www.cancer.gov/about-cancer/coronavirus/coronavirus-cancer-patient-information. Accessed April 2, 2024.
- Hygiene and respiratory viruses prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/hygiene.html. Accessed April 2, 2024.
- Preventing respiratory viruses. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/index.html. Accessed April 2, 2024.
- Maintaining a care plan. Centers for Disease Control and Prevention. https://www.cdc.gov/aging/publications/features/caregivers-month.html. Accessed April 2, 2024.
- COVID-19: What People with Cancer Should Know. National Cancer Institute. https://www.cancer.gov/about-cancer/coronavirus/coronavirus-cancer-patient-information. Accessed April 11, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Coronavirus disease 2019 (COVID-19) - Related information Coronavirus disease 2019 (COVID-19)
- COVID-19 vaccines: Get the facts - Related information COVID-19 vaccines: Get the facts
- COVID-19 Whos at higher risk of serious symptoms
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
- Rare Disease Policy
- Contact NORD
- Show Your Stripes
- Light Up for Rare
- Share Your Story
Faces of Rare
- Attend an Event
- Share an Event
- Meet Our Sponsors
Show Your Stripes ® for Rare Disease Day with NORD
Rare is not rare.
One out of every 10 Americans is living with a rare disease. Worldwide, there are more than 300 million people with rare diseases. Too often, these individuals and families are left isolated and without answers to their medical questions. It doesn't have to be that way. Rare Disease Day is a global initiative to raise awareness and generate support for everyone who is on a rare medical journey. It takes place on the last day of February, which this year is February 29th, the rarest day of the year. The National Organization for Rare Disorders (NORD) is the trusted voice of the more than 30 million Americans living with a rare disease. We are proud to be the official U.S. partner for Rare Disease Day. We invite you to read on to learn how to #ShowYourStripes in support of those with a rare disease.
Show your Stripes®
The zebra is the official mascot for rare disease patients. Historically, medical professionals were told that when they “hear hoofbeats,” they should not expect to see a zebra. In other words, look for the more common answer, a horse. Now, we know that one in ten Americans is actually a zebra! It might not be obvious when you look at us, which is why we show our stripes to raise awareness. Wearing stripes can start a conversation that helps others learn about the prevalence and challenges of rare diseases. Take a picture of your striped look and share it on social media with the hashtags #ShowYourStripes and #RareDiseaseDay to join this celebration of the many faces of rare disease.
- In Your Community
Who do you Show Your Stripes for? We want to hear from you! Behind every face is an extraordinary story and sharing your experience, struggles, and triumphs can help impact change.
Share Your Dedication
Light Up for Rare | International Campaign of Lights
Each year, thousands of buildings, landmarks, homes, and communities around the globe light up in honor of Rare Disease Day. Check out NORD's guide with tips on how to Light Up for Rare and join this global chain of lights.
Find an Event Near You
Share or attend an event.
Rare Disease Day events are happening all month long! Find a local or virtual event to attend or add your own to our calendar.
- Share Event
- Attend Event
Take Action
NORD was founded more than 40 years ago to advocate for equitable health policies that improve the lives of all rare disease patients and families. Advocacy is what Rare Disease Day is all about, and we encourage you to use your own voice today in honor of this moment. Join NORD’s Rare Action Network® to connect with rare advocates near you and take part in our action alerts—sending messages to your representatives about key bills and issues.
- Contact Your Representative
- Join the Rare Action Network
In the News
Everyday hero: milwaukee dad, brewer creates 'zebra hop' beer in honor of his son.
A Milwaukee brewery is working to raise awareness and money to help people living with rare diseases. The cause is personal for Jonathan Kowalske, one of the owners of Component Brewing in the city’s Bay View neighborhood. Shortly after Kowalske opened the business with his two cousins in 2018, his son Mac was born. Mac was diagnosed with Malan Syndrome. To put in perspective just how rare the condition is, Mac is one of only about 200 people worldwide who have been diagnosed with Malan Syndrome.
Rare Disease Day Interview with NORD President and CEO Peter L. Saltonstall and Boston Children’s Hospital’s Dr. Olaf Bodamer
Watch CNBC’s Rare Disease Day interview with NORD President and CEO Peter L. Saltonstall and NORD Rare Disease Center of Excellence Director, Dr. Olaf Bodamer of Boston Children’s Hospital, where they shared how rare disease affects 1 in 10 Americans and why everyone, including the pharmaceutical industry and corporate America, should invest more dollars and attention into rare disease research and treatment.
The IRA needs changes to better support patients with rare diseases
This time last year, members of Congress were working around the clock to draft and pass the Inflation Reduction Act. One of their goals was to address government spending on health care. But they specifically didn’t want to discourage research into rare disease treatments, so they exempted some of these...

IMAGES
VIDEO
COMMENTS
Heart disease is the number one cause of death worldwide. It is caused by a buildup of fatty deposits called plaque in the coronary arteries that supply blood to the heart. This buildup is known as atherosclerosis and can lead to coronary artery disease. Risk factors include age, family history, high cholesterol, smoking, high blood pressure ...
Heart disease. This document provides information about heart disease including: 1. It defines heart disease and lists the common types such as coronary heart disease, hypertension, heart attack, and heart failure. 2. It identifies major risk factors for heart disease such as high cholesterol, hypertension, smoking, diabetes, and obesity. 3.
Heart disease symptoms caused by heart valve problems (valvular heart disease) The heart has four valves — the aortic, mitral, pulmonary and tricuspid valves. They open and close to move blood through the heart. Many things can damage the heart valves. A heart valve may become narrowed (stenosis), leaky (regurgitation or insufficiency) or ...
Arrhythmia refers to an abnormal heart rhythm. There are various types of arrhythmias. The heart can beat too slow, too fast or irregularly. Bradycardia, or a heart rate that's too slow, is when the heart rate is less than 60 beats per minute. Tachycardia, or a heart rate that's too fast, refers to a heart rate of more than 100 beats per ...
Free Google Slides theme, PowerPoint template, and Canva presentation template. Coronary heart disease (CHD) is a very common complication that blocks the arteries of the heart. It is caused by the accumulation of fats in your bloodstream and can cause chest pains, shortness of breath, feeling weak or sick….
Download PowerPoint File. Description: Slides | 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease Date: March 17, 2019 Keywords ...
Heart Arrhythmias. Heart Failure. Heart Valve Disease. Pericardial Disease. Cardiomyopathy (Heart Muscle Disease) Congenital Heart Disease. 4 min read. There are many types of heart disease, and ...
High blood pressure, high blood cholesterol, and smoking are key risk factors for heart disease. About half of people in the United States (47%) have at least one of these three risk factors. Several other medical conditions and lifestyle choices can also put people at a higher risk for heart disease, including. Diabetes. Overweight and obesity
Free Google Slides theme, PowerPoint template, and Canva presentation template. It's time to talk about cardiovascular diseases. Provide some data about them using this creative template full of illustrations of hearts, body diagrams, tables. We have also added useful sections to share data about the diagnosis, recommendations, pathology ...
Valve disease: Tightening or leaking in your heart valves (structures that allow blood to flow from one chamber to another chamber or blood vessel). Coronary artery disease: Problem with your heart's blood vessels, such as blockages. Heart failure: Problem with heart pumping/relaxing functions, leading to fluid buildup and shortness of breath.
Signs and symptoms of coronary artery disease occur when the heart doesn't get enough oxygen-rich blood. If you have coronary artery disease, reduced blood flow to the heart can cause chest pain (angina) and shortness of breath. A complete blockage of blood flow can cause a heart attack. Coronary artery disease often develops over decades.
In general, it's linked with higher cholesterol, higher blood pressure, and an increased risk of heart disease and stroke. Waist circumference also can be a useful tool to measure how much belly fat you have. The risk of heart disease is higher if the waist measurement is greater than: 40 inches (101.6 centimeters, or cm) for men.
Clinical Update Slide Set: 2023 Chronic Coronary Disease Guideline (PPTX) Published: July 20, 2023. Clinical Update Slide Set: 2023 Aneurysmal Subarachnoid Hemorrhage Guideline (PPTX) Published: May 23, 2023. Clinical Update Slide Set: 2022 Aortic Disease Guideline (PPTX) Published: November 2, 2022.
When the heart can no longer do this, blood that. A healthy heart should be able to pump blood to all parts of the body in a few seconds. should be pumped out of the heart backs up in the lungs and other parts of the body. This results is symptoms of heart failure: shortness of breath or swelling in the hands, legs, and feet.
Download ppt "Ischemic Heart Disease". Ischemic heart disease (IHD) represents a group of pathophysiologically related syndromes resulting from myocardial ischemia—an imbalance between myocardial supply (perfusion) and cardiac demand for oxygenated blood. In more than 90% of cases, myocardial ischemia results from reduced blood flow due to ...
Free Google Slides theme, PowerPoint template, and Canva presentation template. Cardiovascular diseases comprehend different cardiopathies. Some of them may lead to heart attacks, strokes or chest pain. Your patients can benefit from your knowledge on them and prevent some of these illnesses with a simple template like this one!
Cardiovascular diseases (CVDs) are the leading cause of death globally. An estimated 17.9 million people died from CVDs in 2019, representing 32% of all global deaths. Of these deaths, 85% were due to heart attack and stroke. Over three quarters of CVD deaths take place in low- and middle-income countries. Out of the 17 million premature deaths ...
The cardiovascular system consists of the heart and blood vessels.[1] There is a wide array of problems that may arise within the cardiovascular system, for example, endocarditis, rheumatic heart disease, abnormalities in the conduction system, among others, cardiovascular disease (CVD) or heart disease refer to the following 4 entities that are the focus of this article[2]:
What is heart disease? Heart disease is a variety of issues that can affect your heart.When people think about heart disease, they often think of the most common type — coronary artery disease (CAD) and the heart attacks it can cause. But you can have trouble with different parts of your heart, like your heart muscle, valves or electrical system.
Download File. ACC.21 Presentation Slides | ISCHEMIA: Completeness of Revascularization in SIHD With Invasive vs. Conservative Strategy. Date: May 17, 2021. Keywords: ACC Annual Scientific Session, ACC21Slides, Dyslipidemias, Geriatrics, Angina, Stable, Percutaneous Coronary Intervention, Angiography. The Image and Slide Gallery captures images ...
Heart Disease. The following presentations provide information on heart disease. The files will download in a Powerpoint presentation format when you click on the title. Alcohol and the Heart. Cholesterol and the Heart. Depression. Exercise and the Heart. Heart Healthy Foods. Stress and the Heart.
Choose healthy food and drinks. Choose healthy meals and snacks to help prevent heart disease and its complications. Be sure to eat plenty of fresh fruits and vegetables and fewer processed foods. Eating lots of foods high in saturated fat and trans fat may contribute to heart disease. Eating foods high in fiber and low in saturated fats, trans ...
Coronary Heart Disease Infographics Download the Coronary Heart Disease Infographics template for PowerPoint or Google Slides and discover the power of infographics. An infographic resource gives you the ability to showcase your content in a more visual way, which will make it easier for your audience to understand your topic.
METHODS: We used nationally representative health, economic, and demographic data to project health care costs attributable to key cardiovascular risk factors (hypertension, diabetes, hypercholesterolemia) and conditions (coronary heart disease, stroke, heart failure, atrial fibrillation) through 2050.
Slide Set | 2020 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease . Print; Download PowerPoint File. Description: See Also: Guideline Hub | Valvular Heart Disease. Date: December 17, 2020
In a report released Tuesday, the American Heart Association says more than 6 in 10 U.S. adults (61%) will have some type of cardiovascular disease, or CVD, by 2050. This is particularly driven by ...
Severe COVID-19 disease is more likely for people who have other health issues. Some common diseases linked to aging are: Heart disease. Examples are heart failure or coronary artery disease. Diabetes mellitus. The risk is higher for both type 1 and type 2. Chronic lung diseases. This includes airway disease and conditions that damage lung ...
Rare Disease Day is a global initiative to raise awareness and generate support for everyone who is on a rare medical journey. It takes place on the last day of February, which this year is February 29th, the rarest day of the year. The National Organization for Rare Disorders (NORD) is the trusted voice of the more than 30 million Americans ...